
Cirugía laparoscópica para próstata
Desde siempre, la glándula prostática ha sido uno de los órganos más intervenidos en varones a partir de la cuarta década de vida, sin embargo, los métodos convencionales como la cirugía abierta traían consigo infinidad de efectos colaterales indeseados que hacían que muchos pacientes se quedaran sin tratamiento mientras las enfermedades avanzaban.
Dentro de los efectos colaterales más frecuentes de las técnicas tradicionales (prostatectomías abiertas) y más temidos por los pacientes se encuentran las disfunciones eréctiles y urinarias, debido al corte de nervios peneanos al extraer la glándula.
No obstante, con el paso del tiempo las técnicas han evolucionado y han aparecido la cirugía robótica de próstata y novedosos abordajes laparoscópicos que producen mínimo daño a los tejidos y estructuras vecinas a la próstata mientras que mejoran notablemente la supervivencia a patologías tan agresivas como el cáncer, en el que es necesario extraer todo el órgano en un procedimiento conocido como prostatectomía.
¿Qué es una prostatectomía?
La prostatectomía es un procedimiento médico de tipo quirúrgico que se realiza como tratamiento a patologías de esta importante glándula masculina, especialmente cuando los tratamientos previos no funcionaron o dicha patología se encuentra en estado avanzado y pone en peligro la vida del paciente.
Esta intervención tiene como objetivo cortar, dividir y extraer una parte de la próstata (conocida como prostatectomía parcial) o bien, extirpar toda la glándula (en un procedimiento llamado prostatectomía total).
La cantidad de tejido resecado (o extirpado) depende de diferentes factores como la edad del paciente y el grado de afección prostática. Asimismo, la prostatectomía contempla además la extracción de ganglios linfáticos adyacentes a la glándula en caso de que algún tipo de cáncer originado en ella los haya podido invadir.
Aunque la prostatectomía tiene excelentes resultados y es una cirugía de dificultad intermedia, los efectos colaterales de las técnicas convencionales la hacen poco atractiva a los pacientes, muchos de los cuales prefieren callar si tienen síntomas de patologías prostáticas y no buscar ayuda médica.
El principal efecto negativo de la prostatectomía está directamente relacionado con la anatomía del órgano. La próstata es un órgano pequeño pero que tiene una ubicación compleja: rodea a la uretra arriba y atrás de la base del cuerpo cavernoso del pene, pegado a la vejiga y rodeado de numerosos nervios encargados de la erección del miembro y de la función urinaria.
Esto dificulta grandemente las operaciones quirúrgicas de la próstata, y ha sido un verdadero desafío a la ciencia médica actual encontrar los métodos menos agresivos con la misma efectividad, que afortunadamente han sido conseguidos, como con la cirugía por medios laparoscópicos con excelentes resultados, especialmente en las prostatectomías radicales por cáncer y tumores prostáticos.
Looking for prices and information?
Use our virtual assistant and receive in your email everything related to the treatments that interest you. Budgets, recovery times, hospitalization, financing possibilities month by month, etc.
In just a few minutes and without any commitment.
En cumplimiento del Reglamento General de Protección de Datos le informamos que los datos por Vd. proporcionados serán objeto de tratamiento por parte de Andromedi con la finalidad de prestarle el servicio solicitado y/o contratado. Los datos no se cederán a terceros salvo en los casos en que exista una obligación legal. Para más información puede consultarla pinchando aquí.
¿Cuándo debe realizarse una prostatectomía radical? ¿Y por qué la laparoscopia es la mejor opción para realizarla?
La prostatectomía radical consiste en la extracción completa de la próstata al existir un proceso neoplásico severo (o hiperplásico) que compromete al órgano y a la salud del organismo en general. La patología que más se beneficia de esta técnica quirúrgica es el cáncer de próstata, también conocido como carcinoma prostático o tumor maligno de próstata.
Tradicionalmente, este procedimiento médico era realizado con la “técnica abierta” donde el cirujano operaba la glándula haciendo primero una incisión de no menos de 10 centímetros en la pared abdominal anterior, a la altura de la pelvis por donde separaba la próstata y la cortaba, dejando libre el trayecto de la uretra pero halando consigo finos nervios del pene.
La cirugía laparoscópica es una técnica novedosa mínimamente invasiva realizada con instrumentos de altísima tecnología que garantizan no solo seguridad sino también efectividad, con efectos colaterales menores y rápida recuperación que llevan a una pronto reinicio de las actividades cotidianas.
La prostatectomía radical con métodos laparoscópicos se indica en pacientes masculinos con cáncer en la porción glandular de la próstata (o adenocarcinoma) y sin metástasis, debido a que esto último implica la invasión a tejidos cercanos como ganglios linfáticos y más dificultad para identificar las estructuras afectadas y extirparlas. Es decir, conlleva un grado mayor de complejidad y por ende, de no una sino varias sesiones de cirugía combinada con tratamientos no quirúrgicos como radioterapia o quimioterapia.
¿En qué consiste la cirugía laparoscópica de próstata?
La prostatectomía laparoscópica es un procedimiento quirúrgico de mínima invasión que se indica para extirpar una próstata invadida por cáncer y que se diferencia principalmente de la cirugía abierta porque solo son necesarias cinco incisiones pequeñas (de menos de un centímetro) en vez de una sola grande.
Esto disminuye el trauma en el abdomen y asegura mejores resultados estéticos y funcionales, con un periodo de recuperación más rápido.
Los hombres sometidos a esta novedosa técnica tienen un menor sangrado, menos dolor y por ende, menos medicación analgésica posquirúrgica, periodos de hospitalización más cortos, rápida reincorporación a la vida cotidiana, pronto retiro de sondas urinarias (que suelen ser incómodas) y en general, una recuperación más rápida que con la cirugía abierta.
¿Cuáles son las ventajas de este procedimiento frente a las técnicas convencionales como la cirugía abierta?
La cirugía abierta para prostatectomía radical o total requiere, por lo mínimo, una incisión abdominopélvica de 20 centímetros mientras que, con laparoscopia solo se necesitan entre cuatro y cinco punto de incisión menor a dos centímetros. Esto hace que el procedimiento tenga una mejor tasa de recuperación, con complicaciones mínimas y dejando una cicatriz casi imperceptible.
- Pérdida mínima de sangre (cerca de 150 ml por lo que no es necesario recibir transfusiones de sangre).
- Estancia en el hospital no mayor a dos días y el paciente puede regresar a casa.
- Menos dolor y riesgo de infección.
- Procedimiento rápido. No suele exceder las dos o tres horas en quirófano.
- El 90 % de los pacientes tienen un regreso más rápido a las actividades cotidianas (entre una y dos semanas) y al trabajo (dos a tres semanas).
Introducción a la Glándula Prostática
Anatomía de la próstata
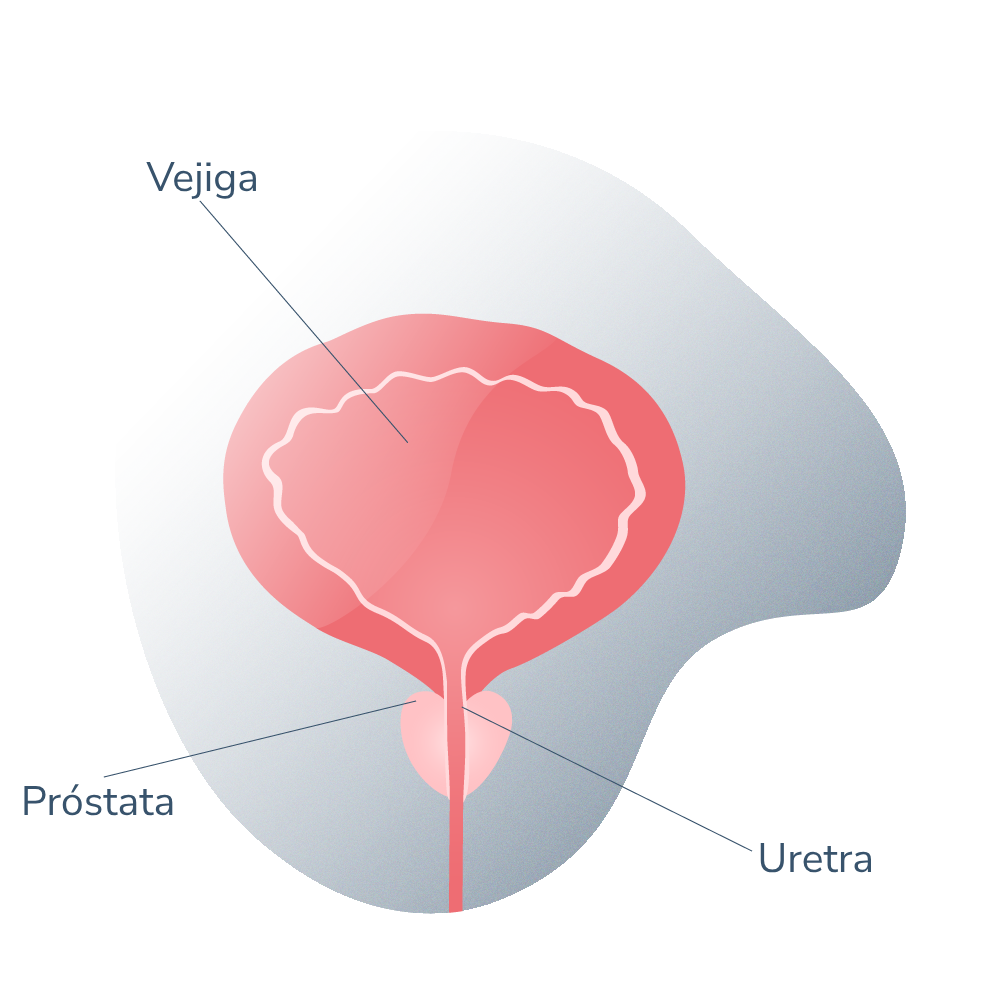
La próstata es un órgano glandular, propio del sexo masculino, que desempeña un importante papel en la reproducción humana del hombre.
Ubicado alrededor de la uretra urinaria, justo por debajo de la vejiga y por delante del recto, la próstata normal posee un tamaño similar al de una nuez. Esta disposición anatómica eleva el compromiso de las vías urinarias si la glándula se ve agrandada o si ocurre hipertrofia.
Función de la próstata
Dentro de las funciones que cumple la próstata se encuentran la secreción de líquido seminal (junto a las vesículas seminales) y la redirección del semen (conjugado con el esperma) en el momento de la eyaculación masculina.
La próstata además, ejerce una función de válvula que impide el paso de orina hacia los testículos (que desencadenaría una infección escrotal, una emergencia urológica) e impulsa el semen cuando se estimula sexualmente y así, producir la eyaculación.
HBP próstata agrandada 01
El semen que es eyaculado contiene una mezcla prácticamente perfecta de sustancias químicas que son necesarias para que los espermatozoides se mantengan con vida dentro del canal vaginal de la mujer y lleven a cabo la posterior fertilización del óvulo. Estas sustancias químicas producidas por la próstata y que soportan los espermatozoides son las siguientes:
- Fructosa, un tipo de azúcar que funciona como un sustento nutricional.
- Fibrinógeno, que le da consistencia al semen (si fuera muy acuoso tendría dificultades para mantenerse en la cavidad femenina).
- Enzimas necesarias para la fertilización del óvulo.
- Agentes antibióticos.
Las funciones secretoras de la glándula están reguladas por factores hormonales andrológicos, de los cuales, la testosterona lleva el rol más fundamental.
¿Por qué enferma la próstata?
Los tejidos prostáticos están compuestos por células con alto número de receptores para la testosterona y que reaccionan ante los niveles sanguíneos circundantes de esta hormona.
Sin embargo, con el paso de los años y con el conjunto de cambios hormonales propios del envejecimiento (los niveles de testosterona en sangre decaen por una baja producción de la misma en las células de Leydig en los testículos), los tejidos de la glándula se hacen hipersensibles a la hormona haciendo que esta se agrande o hipertrofie excesivamente. A esto se le conoce como hiperplasia benigna de próstata (HBP), que se trata con medicamentos que reducen el número de receptores androgénicos, y por ende, la sensibilidad a estas hormonas. Esta patología masculina es muy frecuente en hombres mayores a partir de la cuarta década de vida.
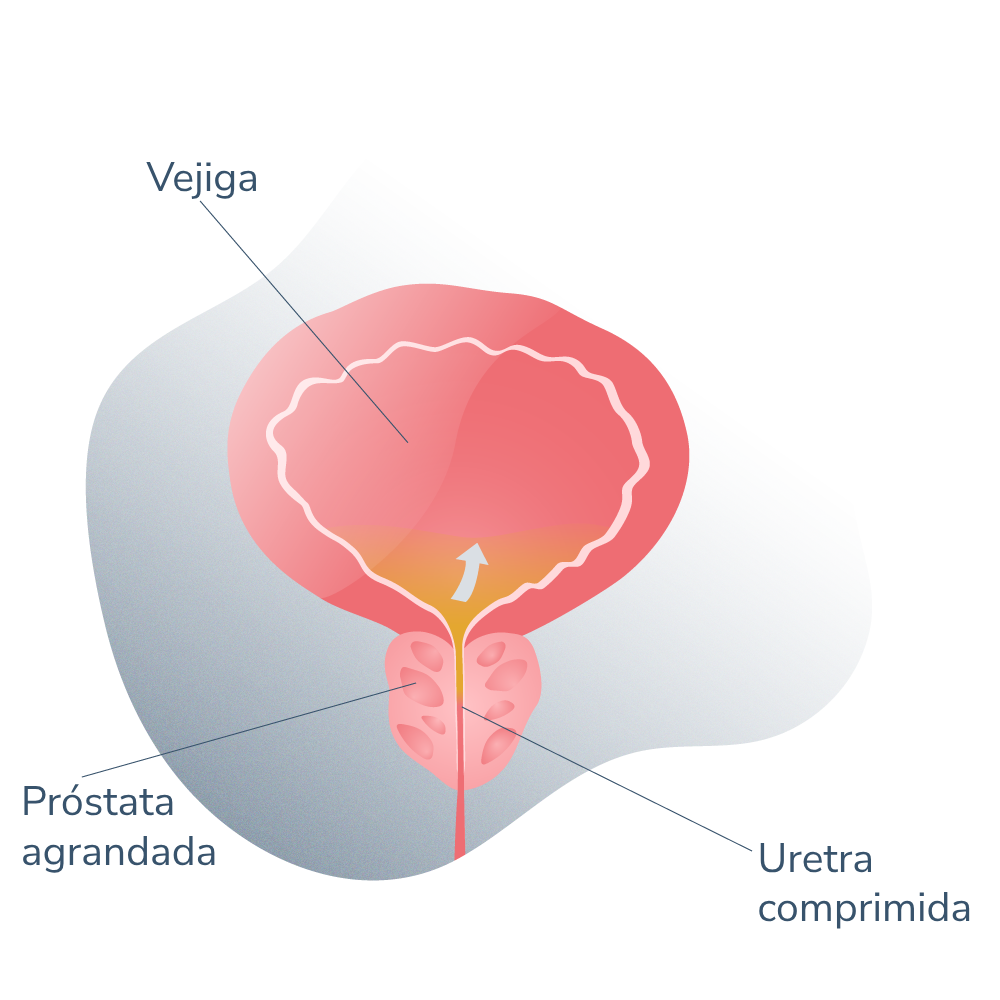
HBP próstata agrandada 02
Por otro lado. Existen patologías más agresivas que también tienen alta prevalencia, como el cáncer de próstata, de la que hablaremos con más detalle más adelante.
Cáncer de próstata
El cáncer de próstata es por mucho, la neoplasia maligna más frecuente en hombres de edades adultas avanzadas. Se trata de la malignización progresiva de los tejidos prostáticos que cursa además, con el agrandamiento de la próstata dificultando la micción y el incremento del riesgo de invasión a tejidos vecinos (o metástasis) si no es tratado oportunamente.
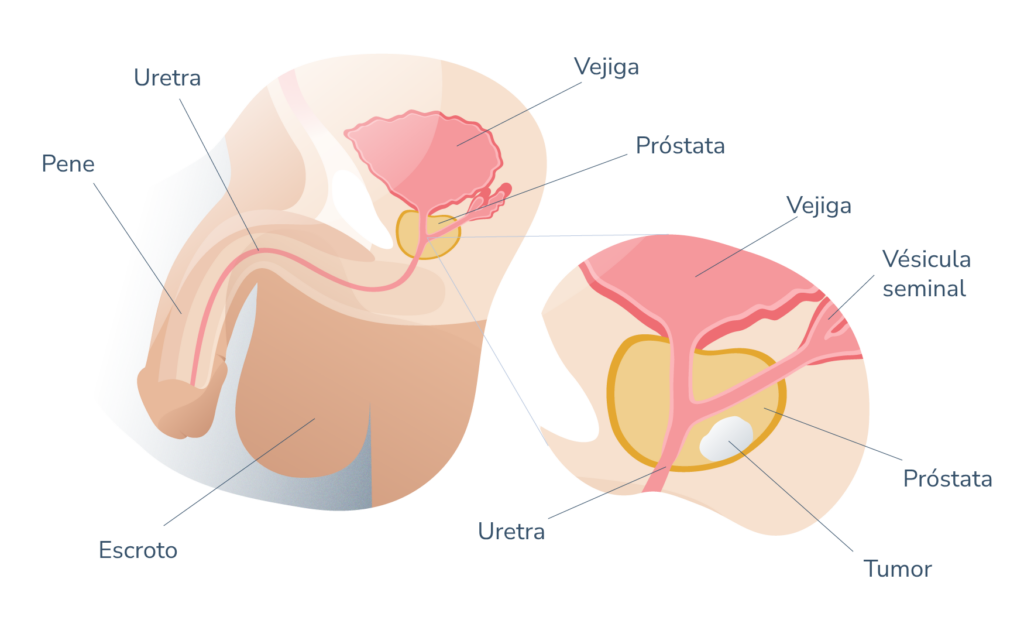
Anatomía general de la próstata 01
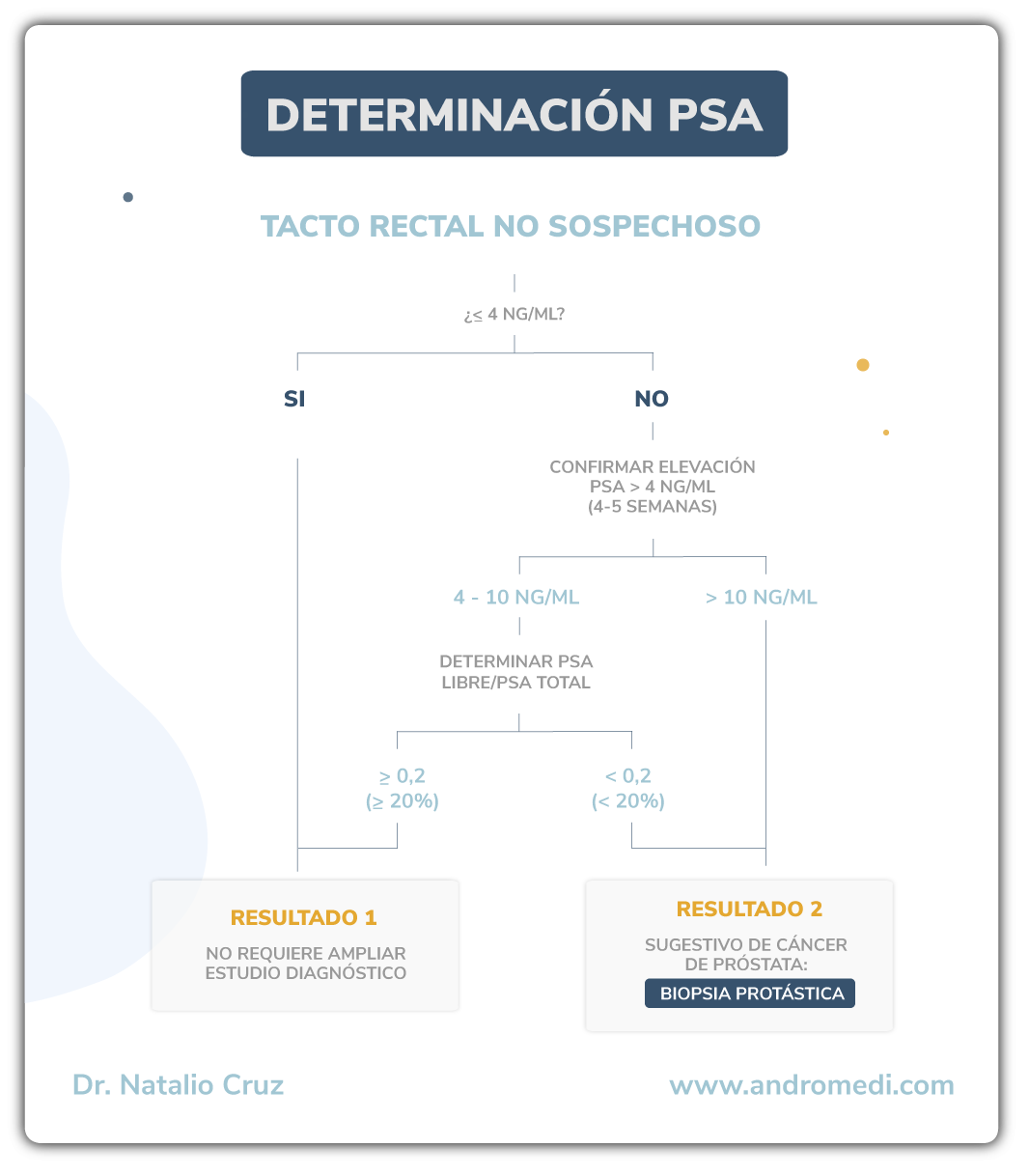
El éxito del tratamiento contra el cáncer de próstata es directamente proporcional a la fase en la que es detectado. El diagnóstico del cáncer de próstata comienza con la detección de un agrandamiento de próstata a través de un examen físico conocido como tacto rectal digital.
El tacto rectal digital y el análisis de los niveles sanguíneos de antígeno prostático (PSA) han sido la piedra angular de una sospecha de agrandamiento de próstata. El diagnóstico del cáncer se realiza en base a una minuciosa revisión de los antecedentes personales y familiares del paciente, la exploración física y la realización de una biopsia, hoy dia guiada por fusión con imágenes de ecografía.
Procedimiento y técnica ¿en qué consiste?
Preparación previa
Antes de la intervención quirúrgica, el cirujano realiza una serie de consultas para examinar al paciente y pedir estudios por imágenes como resonancias y ecosonogramas. Esto sirve para evaluar el estado de la próstata y prever cómo será la cirugía. También se indican algunos exámenes de sangre para determinar la química sanguínea por medio de un hemograma.
Dependiendo del paciente y de sus patologías previas (como síndrome coronario, patologías valvulares, hipertensión arterial o angina de pecho) es posible que el médico también indique un electrocardiograma o un examen de función pulmonar que permitan evaluar el estado de salud del paciente.
Aunado a esto, también se recomienda que el paciente modifique algunos hábitos y estilos de vida como:
- Dejar de consumir fármacos anticoagulantes como la aspirina o la warfarina (o cualquier otro similar).
- Dejar de consumir analgésicos y antiinflamatorios no esteroideos
- Mantener una dieta líquida o semilíquida en las 24 horas anteriores a la cirugía.
- Pasada la medianoche del día anterior a la cirugía, se recomienda tomar muy poco líquidos. Unos cuantos y pequeños sorbos de agua serán suficientes para calmar la sed si llegara a aparecer.
- Probablemente también se indique la abstinencia de alcohol, tabaco y cualquier tipo de narcótico. Dejar de fumar es clave para ayudar a que el cuerpo y los tejidos manipulados en la cirugía perciban mejor riego sanguíneo y aporte de oxígeno para acelerar el proceso de recuperación.

¿Cómo es la anestesia para la cirugía?
La anestesia que se requiere en este tipo de intervención quirúrgica es la anestesia general dado la anatomía del abdomen y la pelvis, que contienen abundantes tractos nerviosos importantes. Esto asegura que el procedimiento sea totalmente indoloro.
Antes de la intervención, el paciente debe reunirse con el especialista en anestesiología, se realizan algunas pruebas para determinar el tipo de anestesia adecuado al paciente, en cuanto a fármaco y dosis. También sirve para descartar cualquier hipersensibilidad a la misma.
Durante la cirugía: el paso a paso
El equipo de cirujanos realiza algunas incisiones en el abdomen, generalmente entre cuatro y cinco incisiones de dos centímetros aproximadamente. Por estos orificios serán insertados los instrumentos quirúrgicos necesarios para la resección total de la glándula y una cámara de vídeo que servirá para mostrar la ejecución del procedimiento en un monitor de TV.
Una vez realizados los orificios hacia la cavidad pélvica, el cirujano urólogo procede a:
- A través de uno de los orificios realizados (ubicado cerca del ombligo) se introducirá una muy delgada cánula encargada de inyectar dióxido de carbono dentro de la cavidad abdominal con el fin de levantar la pared del abdomen y ampliar así el campo de visión del cirujano.
- Separar la próstata de los tejidos vecinos, especialmente de los tejidos conjuntivos de sostén adheridos a ella.
- De no ver nada anormal o patológico, el cirujano accede con sus instrumentos especializados hasta el lugar de la posición anatómica de la próstata, por debajo de la vejiga urinaria. Si es necesario, se cortan algunas capas de tejido profundo para acceder hasta los ganglios linfáticos que drenan la linfa de la próstata porque pudieran estar invadidos por células cancerosas.
- Se separa cuidadosamente la próstata de los tejidos vecinos, especialmente de los tejidos conjuntivos de sostén que están adheridos a ella y de los nervios que van al pene.
- Cortar los vasos sanguíneos y nervios que van a la glándula.
- Cortar el pedículo de fijación a la vejiga urinaria y a la uretra (la porción prostática de la uretra es extirpada completamente).
- Se extrae la próstata y las vesículas seminales.
- Se reconecta el extremo superior de la uretra con la porción inferior de la vejiga.
- Se suturan los orificios de entrada de los instrumentos laparoscópicos.
Es probable que se extraigan también algunos ganglios linfáticos para estudios y biopsias.
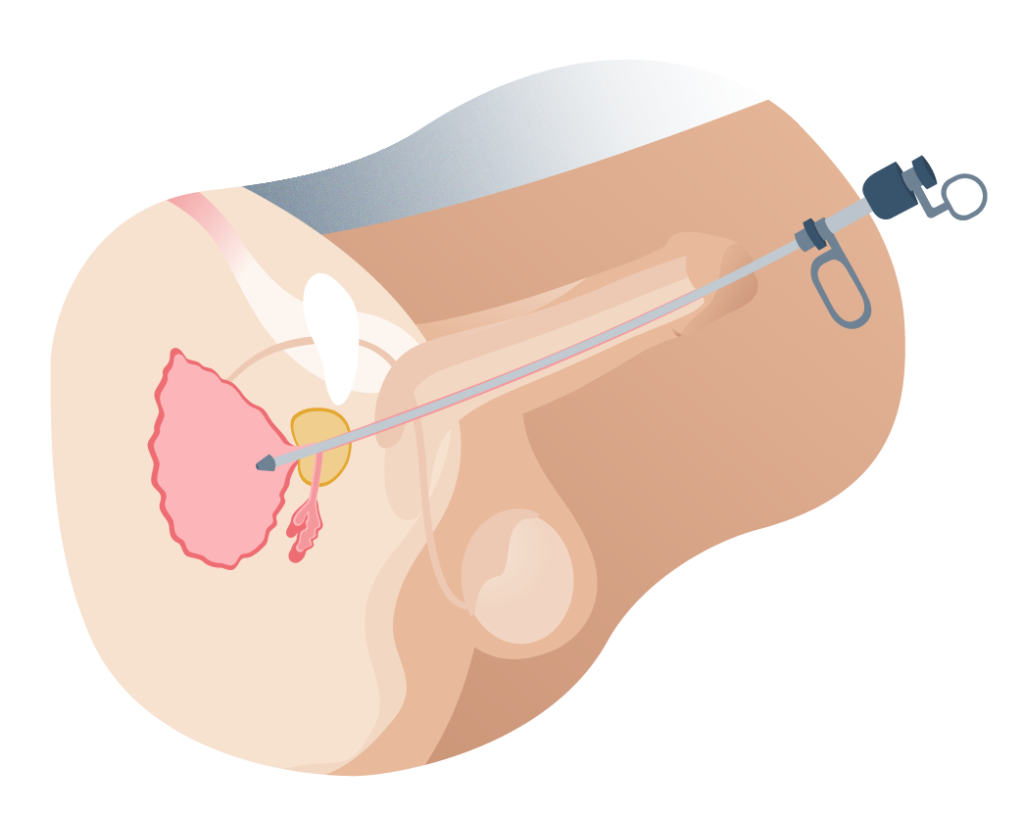
Cirugía próstata por laparoscopia
Cuidados para después de la cirugía prostática por laparoscopia
Después de la cirugía los médicos mantendrán al paciente durante dos o tres días en el hospital para monitorear su progreso y prevenir cualquier complicación que pudiera desarrollarse.
Durante este periodo de hospitalización, se recomienda que el paciente haga caminatas cortas y lentas para mejorar la circulación sanguínea en la parte baja del cuerpo y se promueva la reparación de los tejidos.
- Además, la dieta del paciente será líquida o semilíquida. Progresivamente se irán incorporando alimentos más sólidos hasta restablecer por completo la alimentación habitual del paciente según indicaciones del médico tratante.
- Es completamente normal que después de un procedimiento quirúrgico de este tipo los pacientes sientan náuseas y vómitos porque los intestinos se detienen temporalmente por la anestesia utilizada. Esto es benigno y desaparece por sí solo antes de las 24 horas.
- También se indican medicamentos para aliviar el dolor postoperatorio y antibióticos para prevenir posibles infecciones.
- El paciente debe permanecer dos o tres semanas de reposo físico en casa, cuidando de no realizar ejercicio físico extenuante o levantar pesadas cargas. Se recomienda que el paciente camine un poco más cada día para aumentar el riesgo sanguíneo hasta volver a desempeñar las actividades cotidianas.

La idea de todo este tiempo de recuperación cuidadosa es que el paciente logre retornar progresivamente a su vida cotidiana sin sobrecargar al organismo con grandes esfuerzos físicos que podrían, entre otras cosas, lastimar los tejidos intervenidos y complicar el pronóstico.
Prostatectomía radical por laparoscopia robótica ¿cuál es la diferencia con la laparoscopia tradicional?
La laparoscopia tradicional y la laparoscopia robótica se fundamentan en la misma técnica: un conjunto de aparatos quirúrgicos introducidos en alguna cavidad y una cámara de vídeo que ayude a observar el procedimiento. La diferencia entre estas dos variantes radica en el instrumentista.
En la cirugía laparoscópica tradicional, los cirujanos ejecutan las técnicas y procedimientos en el sitio mismo, manipulando los instrumentos ellos mismos. Se requieren entre dos y tres cirujanos en quirófano para ejecutar coordinadamente la intervención.
Con la laparoscopia robótica (o asistida por robot) el cirujano se sienta frente a un panel de controles y con ayuda de un monitor de TV va moviendo los instrumentos dentro del cuerpo del paciente. El sistema tiene brazos robóticos y se mueven en concordancia con los movimientos del médico.
En esta última técnica, se requiere el médico cirujano cuente habilidades específicas para esta técnica, la cual ofrece mejores resultados aún, que la laparoscopia tradicional.

¿Cuáles son los resultados?
Se calcula que el 97 por ciento de los pacientes con carcinoma prostático localizado alcanzan resultados positivos posteriores a una prostatectomía radical laparoscópica. Evidentemente estos resultados pueden variar de paciente a paciente a la cantidad de tejido prostático extirpado. En algunos casos de extraen tejidos adyacentes a la próstata como tejido graso, vesículas seminales y algo de uretra o vejiga urinaria.
¿Cuánto tiempo dura la cirugía de prostatectomía por laparoscopia?
El tiempo requerido para ejecutar una prostatectomía radical por laparoscopia puede variar de entre 2 horas 30 minutos y 3 horas 30 minutos dependiendo de la anatomía de cada individuo, el tamaño de la próstata y si es requerido extirpar otros tejidos circundantes.
La mayoría de los pacientes pueden regresar a casa el día siguiente a la intervención por lo que la estancia hospitalaria es mínima, aunque si se requiere reposo en casa. Dos o tres semana son suficientes para regresar a las actividades cotidianas por completo. Será el médico tratante el encargado de indicar cuanto tiempo es necesario con base a los chequeos posquirúrgicos.
Otro factor importante es la colocación de un catéter para orinar sin forzar la uretra posterior a la cirugía.
Con las técnicas convencionales (cirugía abierta) el catéter debe permanecer dentro de la uretra peneana del paciente durante unas dos o tres semanas dado que el grado de trauma en los tejidos fue mayor.
No obstante, con la cirugía laparoscópica de próstata es posible retirar el catéter vesical (mejor conocido como sonda de Foley) el tercer día después de la intervención.
Preguntas frecuentes acerca de la cirugía prostática
Hide
- Sangre en la orina (hematuria).
- Infecciones, especialmente de tracto urinario (ITU).
- Dolor post quirúrgico, que se trata con analgésicos.
- Hematomas en los sitios cercanos a los orificios de la laparoscopia.
Los hombres sometidos a prostatectomías laparoscópicas vuelven a gozar de una función urinaria completamente normal y voluntaria, sin incomodidades o signos de obstrucción, pasados unos tres meses después de la cirugía.
Hay que tener en cuenta el importante porcentaje de pacientes que, a causa de los trastornos prostáticos (como la hiperplasia benigna de próstata o los tumores malignos de la glándula) perdieron la capacidad de orinar con tranquilidad, así que tres meses es un tiempo más que positivo para recuperar esta función.
Después de la cirugía, el médico dará indicaciones específicas sobre el cuidado del sitio de la operación para acelerar el proceso de recuperación y cicatrización. Más específicamente, de las incisiones que fueron realizadas en la piel y, para ello, los cuidados son los siguientes:
• Colocar adhesivo estéril, especial para estos casos, en el sitio de las incisiones durante unos 10 días a dos semanas después de la intervención. Esto ayudará a que cada incisión permanezca lo más seca, limpia y protegida posible del roce de la ropa.
• Evitar tomar aspirina para tratar el dolor, en ese caso, es posible tomar analgésicos sin receta como el acetaminofén.
• Es normal que la piel cercana a los sitios de incisión cambie de color y se torne un poco azulada u oscura. Esto es completamente normal y desaparecerá por sí solo al cabo de un par de días.
• Cuándo volver a conducir un coche es una pregunta frecuente entre los hombres sometidos a esta cirugía y la verdad es que no existe un tiempo establecido, pero en la mayoría de los pacientes pueden volver a hacerlo en unos 10 a 14 días. Todo esto depende de las indicaciones del médico.
 La disfunción eréctil (DE) representa el riesgo más importante y con mayor prevalencia que se corre al realizar una prostatectomía radical, sea cual fuere su modalidad quirúrgica.
Evidentemente, los médicos guardan mucho cuidado al realizar la extirpación de la próstata y de dejar intactos el conjunto de nervios que inervan al pene y las estructuras genitales. Sin embargo, la anatomía indica que existe una estrecha relación entre la glándula y estos nervios, por lo que al extraerlo también se lleva consigo algo de nervios, disminuyendo la sensibilidad de la zona y la respuesta eréctil de los cuerpos cavernosos.
No obstante, no todo está perdido. Si ocurre impotencia sexual masculina, disfunción eréctil o erecciones débiles pueden recurrirse a otros métodos terapéuticos para mantener la vida sexual activa de los pacientes. Estos métodos terapéuticos incluyen:
La disfunción eréctil (DE) representa el riesgo más importante y con mayor prevalencia que se corre al realizar una prostatectomía radical, sea cual fuere su modalidad quirúrgica.
Evidentemente, los médicos guardan mucho cuidado al realizar la extirpación de la próstata y de dejar intactos el conjunto de nervios que inervan al pene y las estructuras genitales. Sin embargo, la anatomía indica que existe una estrecha relación entre la glándula y estos nervios, por lo que al extraerlo también se lleva consigo algo de nervios, disminuyendo la sensibilidad de la zona y la respuesta eréctil de los cuerpos cavernosos.
No obstante, no todo está perdido. Si ocurre impotencia sexual masculina, disfunción eréctil o erecciones débiles pueden recurrirse a otros métodos terapéuticos para mantener la vida sexual activa de los pacientes. Estos métodos terapéuticos incluyen:
- Fármacos inhibidores de la fosfodiesterasa 5, mejor conocidos como retardantes del tipo sildenafilo, taladafilo o vardenafilo. Generalmente vía oral, en comprimidos.
- Inyecciones intracavernosas de fármacos vasodilatadores, con excelentes resultados a corto y mediano plazo.
- Bombas de succión o al vacío.
- Implantes de pene.
No, debido a que la próstata que será eventualmente extraída no tiene como función la producción de espermatozoides (esto ocurre en los testículos, dentro del escroto).
Después de la cirugía, las eyaculaciones serán un poco menos abundantes (porque la próstata produce parte del semen) pero la capacidad de fertilizar sigue intacta a menos que haya problemas en los testículos.
Si te encuentras en el periodo de recuperación y notas los siguientes síntomas es importante llamar al médico o acudir a consulta:
• Fiebre mayor de 40° C.
• Si el dolor es muy fuerte o no desaparece con los analgésicos indicados.
• Dificultad para orinar o sangre en la orina.
• Mareos y vértigo.
Sí, es necesario usar catéter o sonda vesical durante algún tiempo posterior a la cirugía de prostatectomía radical debido a que se requiere dar oportunidad a los tejidos uretrales a que se reconecten y cicatricen. Generalmente se requieren entre dos y tres semanas con sonda.
Todo paciente masculino con diagnóstico de cáncer de próstata localizado sin metástasis puede ser candidato a la prostatectomía radical laparoscópica.
No obstante, cada caso debe ser atendido y valorado de manera individual puesto que en contados casos, un tumor no tan bien localizado dentro del tejido glandular prostático puede ser abordado por métodos laparoscópicos.
Los médicos recomiendan abstinencia sexual absoluta durante un mes después de una intervención de este tipo. Esta abstinencia incluye relaciones sexuales con penetración, masturbación y eyaculación (la eyaculación podría ser dolorosa o con algo de sangre).
Desarrollar problemas eréctiles menores después de haber sido eliminado un órgano potencialmente peligroso para la vida del paciente es algo menor. De hecho, es algo infrecuente con esta técnica y los hombres siguen gozando de una vida sexual activa y plena.
En muchos otros casos, la disfunción eréctil ya era un problema de base. Es decir, ya estaba presente antes de la cirugía (especialmente en pacientes obesos, diabéticos, hipertensos o de edad muy avanzada).
Dentro de las alternativas para tratar la disfunción eréctil se encuentran:
• Medicamentos inhibidores de la fosfodiesterasa 5 como el sildenafilo, el taladafilo o el vardenafilo que favorecen la relajación de los vasos sanguíneos que van al pene y por ende, los mecanismos de la erección se potencian.
• Inyecciones intracavernosas de alprostadil, un medicamento con efecto vasodilatador que se infiltra en la base de los cuerpos cavernosos del pene y tiene un efecto prolongado.
• Bombas de vacío, unos dispositivos de succión en los que se inserta el pene en estado de flacidez para inducir la erección.
• Cirugía de implantes peneanos, una solución definitiva y quirúrgica al problema.
Referencias médicas y bibliografía
- ¿Qué es el cáncer de próstata? American cancer society
- Carcinoma prostático Manual msd para profesionales
- Cirugía para el cáncer de próstata American cancer society
- La laparoscopia ofrece alta precisión a la prostatectomía radical El médico interactivo web
- Prostatectomía radical laparoscópica: revisión en la literatura médica Scielo
BLOG ANDROMEDI
Otros artículos que te pueden interesar

Laparoscopic surgery for prostate
26 September 2023

Laser prostate surgery
22 November 2021

Impotence, incontinence and other problems after prostate surgery
22 November 2021
Author
El Dr. Juan Manuel Poyato, con más de 15 años de experiencia médica, es especialista en Urología, Medicina Sexual y Andrología, Es Profesor Externo del Departamento de Fisiología Médica y Biofísica de la Universidad de Sevilla y Coordinador de Urología de la Agencia Sanitaria Bajo Guadalquivir de la Consejería de Salud (Junta de Andalucía).

