TREATMENTS for Prostate Problems
Prostatitis
Prostatitis is an acute, inflammatory disorder of the prostate gland. It is characterised by bothersome urinary symptoms such as painful urination, burning in the urethra and even pelvic pain. Treatment may consist of specific antibiotics, non-steroidal anti-inflammatory drugs, urinary antiseptics and in extreme cases surgery is indicated, depending on the type of prostatitis.
- VÍDEO: La próstata, esa gran desconocida - Canal Sur Radio
Prostatitis
Table of content
- VÍDEO: La próstata, esa gran desconocida - Canal Sur Radio
Chances of developing prostate cancer
Introduction to prostatitis
Prostatitis is an acute inflammatory disorder of the prostate gland, almost always related to infectious processes that are characterized by annoying urinary symptoms such as pain when urinating, burning in the urethra and even pain in the pelvis.
The reasons why a prostate becomes inflamed can be quite diverse such as bacterial infections of the gland, trauma or blows that affect the prostate or muscle spasms of the pelvic floor (or urogenital diaphragm).
Anatomía general de la próstata
The diagnosis of this disease is usually made by the clinic that the patient presents without so many complementary studies, although carrying out laboratory analysis can be really useful to elucidate what type of pathogen could be causing the infection and which antibiotic would be the correct one to combat it. , for example.
The treatment of prostatitis is almost always pharmacological, with antibiotics for bacterial prostatitis and with warm sitz baths, drugs to relax the muscles, and anti-inflammatory drugs for non-bacterial prostatitis.
Looking for prices and information?
Use our virtual assistant and receive in your email everything related to the treatments that interest you. Budgets, recovery times, hospitalization, financing possibilities month by month, etc.
In just a few minutes and without any commitment.
En cumplimiento del Reglamento General de Protección de Datos le informamos que los datos por Vd. proporcionados serán objeto de tratamiento por parte de Andromedi con la finalidad de prestarle el servicio solicitado y/o contratado. Los datos no se cederán a terceros salvo en los casos en que exista una obligación legal. Para más información puede consultarla pinchando aquí.
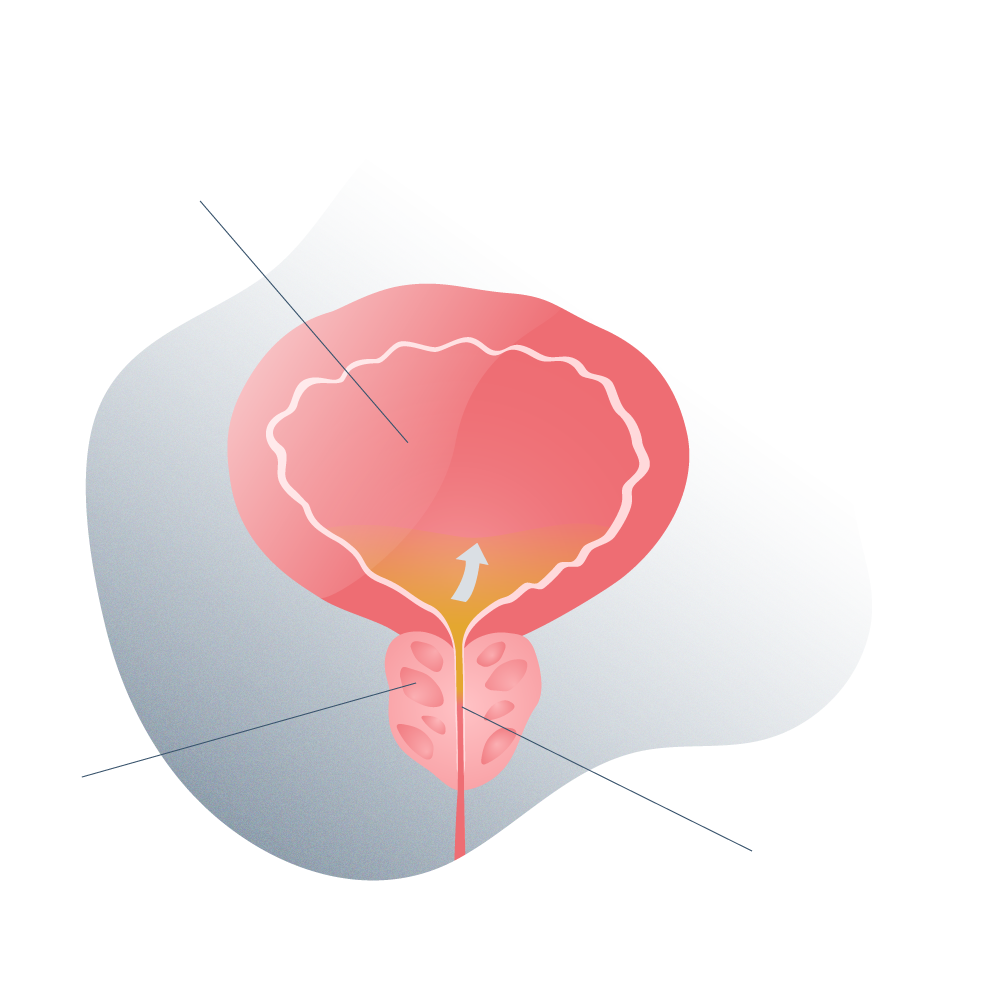
Where is the prostate located?
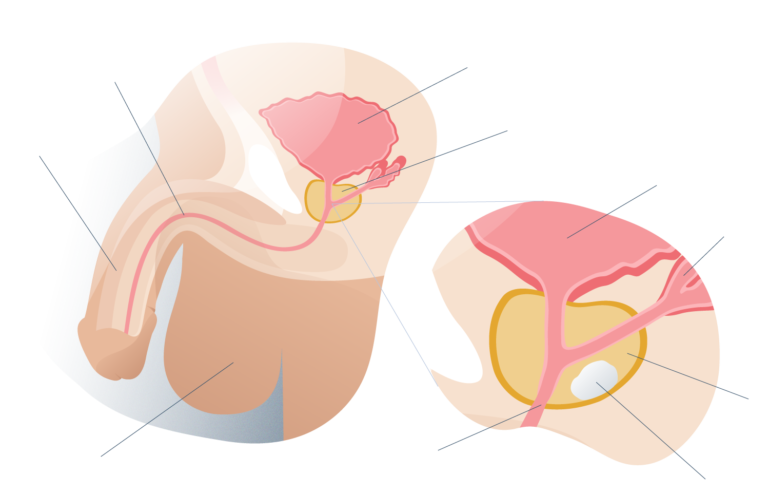
General anatomy of the prostate
The prostate is a gland the size of a walnut (as it was described by the first anatomists in the Middle Ages) that is located in the pelvic region of man.
This gland has an oval shape and is slightly elongated to the sides. It is located just below the urinary bladder and surrounds the first portion of the urethra.
The urethra is the tube through which urine flows from the bladder (the storage site for urine produced in the kidneys) to the opening of the glans at the tip of the penis. This transport of urine occurs only during voluntary urination and any unwanted loss of urine is considered incontinence and is a pathology.
But the prostate is not only related to urinary function but also to sexual function because the sperm ducts of both testicles lead to the prostatic urethra, where they combine with the seminal fluid produced by the prostate at the time of ejaculation.
Outside the prostate and attached to it are many nerves that go to the penis and whose function is to produce and maintain the erection of the member until after ejaculation. If the gland grows too large and compresses these nerves, or if these nerves are injured during surgery, the patient could develop erectile dysfunction or ED.
What does the prostate do?
The prostate has three essential functions, some more important than others, but without a doubt, all important for urinary function and sexual function.
These functions are:
A Production of seminal fluid: the prostate is responsible for synthesizing a large part of the semen that, during ejaculation, is expelled from the man’s body. Semen is a viscous fluid that combines with sperm and has the ability to nourish and protect sperm during their passage from the vaginal canal to the site of fertilization with the egg.
B The prostate acts as a pump that helps expel seminal fluid during ejaculation (the point of maximum sexual arousal in men).
C The prostate acts as a valve that directs the flow of seminal fluid towards the penis, thus preventing the retrograde flow of semen to the urinary bladder during ejaculation.
How common are prostatitis?
The prevalence of prostatitis can vary depending on the region of the world where it is investigated. In regions such as Europe and Latin America, the prevalence of this disease is around 2 to 16% of men of reproductive age, thus constituting 8% of all urology consultations.
Although it may seem an insignificant number, inflammation of the prostate should arouse interest in healthy patients and individuals for two essential reasons:
A In most cases, prostatitis can be prevented.
B In most cases, prostatitis usually has a good prognosis if correct and timely treatment is applied (for this it is necessary to visit the urologist).
C c) If prostatitis is not treated, it can cause serious complications, some of them irreversible and potentially fatal.
Why do prostate problems affect so much?
Prostatitis or inflammation of the prostate like any other pathology related to this important male gland significantly affect the quality of life of the man who suffers from it because the rate of complications is high if it is not treated in time.
However, this is where the origin of the problem lies: many men who notice urinary symptoms do not go to the doctor or ask for professional help out of embarrassment.
The prostate is a gland in close anatomical and functional relationship with the urinary system and the reproductive system. If any increase in volume occurs (whatever the cause, infection, trauma, hiperplasia a or cancer), the prostate will compress the tube through which urine and semen flow.
In the long term, if prostate tissue dies or becomes dysfunctional, semen production will suffer and with it, the ability to have children.

TREATMENTS
Types of prostatitis and how to tell if I have prostatitis

Understanding that prostatitis is a condition with different causes, also the symptoms that each type of prostatitis produces is different from the others and this is quite useful for the urologist who is diagnosing inflammation.
The main types of prostatitis and their symptoms are:
Chronic bacterial prostatitis
This type of bacterial prostatitis is rare because generally, bacterial infections are successfully treated with antibiotics or the immune system fights them off within a few weeks or days.
Unless the patient has a strong immune system or seeks medical help at the first symptoms of pelvic infection, it is possible to develop chronic prostatitis.
To diagnose this type of prostatitis, it is necessary to perform urine and prostate fluid cultures. Most patients with chronic bacterial prostatitis report that “symptoms come and go” for long periods of time, but when they are not present, they are unconcerned and believe that the disease has resolved itself.
Bacteria that invade prostate tissues may lie dormant for a long time before reoccurring symptoms.
Among the most common symptoms of this type of prostatitis we find:
- Burning in the urethra and penis when urinating
- Sensation of wanting to urinate constantly.
- Feeling of (incomplete emptying of the bladder).
- Pain in the pelvic region that can extend to the testicles, penis, and anus (this indicates a severe infection).
- Severe pain during ejaculation.
Sometimes the burning when urinating can be so strong that the patient has to stop urination until it is relieved but it can appear again when urinating again.
Acute bacterial prostatitis
Like the previous one, it is also a rare type of prostatitis but it can happen, especially in men who have constant urinary infections. Urine cultures are necessary to determine the pathogen (generally Escherichia coli in 80% of cases) and which is the ideal antibiotic.
The symptoms of acute bacterial prostatitis are quite sudden and appear very intensely without warning. This causes many patients to go to the doctor immediately.
Symptoms of this type of prostatitis include:
- Fever greater than 39 ° C and chills.
- General discomfort.
- Loss of appetite.
- Intense burning when urinating.
- Difficulty starting to urinate..
- Difficulty emptying all the contents of the bladder (the patient feels that he did not urinate completely).
In some cases, the sensation of not having urinated all the contents of the bladder is so stressful that it is necessary to indicate anxiolytics. No one is prepared for the discomfort of not being able to urinate properly, many patients develop nervousness and avoid situations that involve leaving the house or not having a bathroom nearby.
Chronic pelvic pain syndrome (CPPS) due to prostatitis
Chronic prostatitis or better known as chronic pelvic pain syndrome (CPPS) is the most common type of non-infectious inflammation of the prostate. It is very painful because inflammation of the prostate tends to irritate the nerves that surround the gland.
Symptoms of chronic pelvic pain syndrome due to non-infectious prostatitis are:
- Moderate burning when urinating..
- Constant need to urinate and a feeling of not having completely urinated (incomplete bladder emptying).
- Pain in the entire pelvic area of the man: bladder, urethra, testicles, penis and anus (and the region between the latter two).
- Very painful ejaculation.
Asymptomatic inflammatory prostatitis
This type of prostatitis, as its name implies, is a real inflammation of the prostate due to non-infectious causes that does not generate pain and therefore, can go unnoticed.
But how is this possible? The prostate can enlarge (become inflamed) from a blow during a soccer game, for example, but in some men, the prostate does not compress or irritate the nerves located around it and for this reason, the patient does not notice the inflammation.
In most cases, the prostate loses its swelling on its own within a few days.
Often times, some patients come to routine consultations to our clinics in Madrid, Seville and Tenerife and upon a digital rectal examination, the prostate appears enlarged but infection, hyperplasia, and even a malignant tumor are quickly ruled out.
"Treatment of prostatitis is almost always pharmacological, with antibiotics for bacterial prostatitis and warm sitz baths, muscle relaxants and anti-inflammatory drugs for non-bacterial prostatitis".
What is prostatitis?
Treatment Summary
Prostatitis can be caused by infections (bacterial or non-bacterial) but also by other non-infectious causes such as trauma to the gland, kidney stones that may have irritated the prostate during its passage through the urethra, intense prostate massages and even certain surgical interventions or diagnostic. to receiving the medical discharge after the treatment in some our Andromedi centers in Madrid, Seville or Canary islands (Tenerife)
What causes prostatitis?
Prostatitis can be caused by infections (bacterial or non-bacterial) but also by other non-infectious causes such as trauma to the gland, kidney stones that may have irritated the prostate during its passage through the urethra, intense prostate massages and even certain surgical interventions or diagnostic.
How is it diagnosed?
By means of a medical interview and a physical examination, with an emphasis on a digital rectal examination. Urine or prostate discharge tests, ultrasound scans, cystograms, and urodynamic tests are also helpful.
Treatments of prostatitis
Treatment depends on the type of prostatitis. If it is infectious, treatment consists of specific antibiotics for the bacteria causing the problem. Nonsteroidal anti-inflammatory drugs, urinary antiseptics, and consuming large amounts of fluid can also help. In extreme cases, surgery (prostate abscess) is indicated.
Symptoms of prostatitis
Prostatitis is characterized by producing obstructive symptoms in the lower urinary tract such as difficulty urinating, burning when urinating, pain in the pelvic region and even severe discomfort when ejaculating. Some prostatitis may be asymptomatic.
What happens if it is not treated?
Almost always, prostatitis usually have a good prognosis but if they are not treated promptly (being infectious) and the patient also has a weakened immune system, prostatic abscesses can develop.
Treatment
Treatment: How is prostatitis solved?
The clinical management of prostatitis depends directly on the type of it, for example:
Acute bacterial prostatitis
With this type of prostatitis, the patient requires to consume antibiotics (prescribed by a doctor) for at least two weeks. Regarding the presentation of the drug, intravenous administration is recommended to ensure the action of the antibiotic at the site of infection.
If the patient reports difficulty urinating, it is advisable to place a urinary catheter to drain urine and prevent a dangerous pressure overload on the kidneys (a pathology known as hydronephrosis due to urethral obstruction that can cause kidney damage).
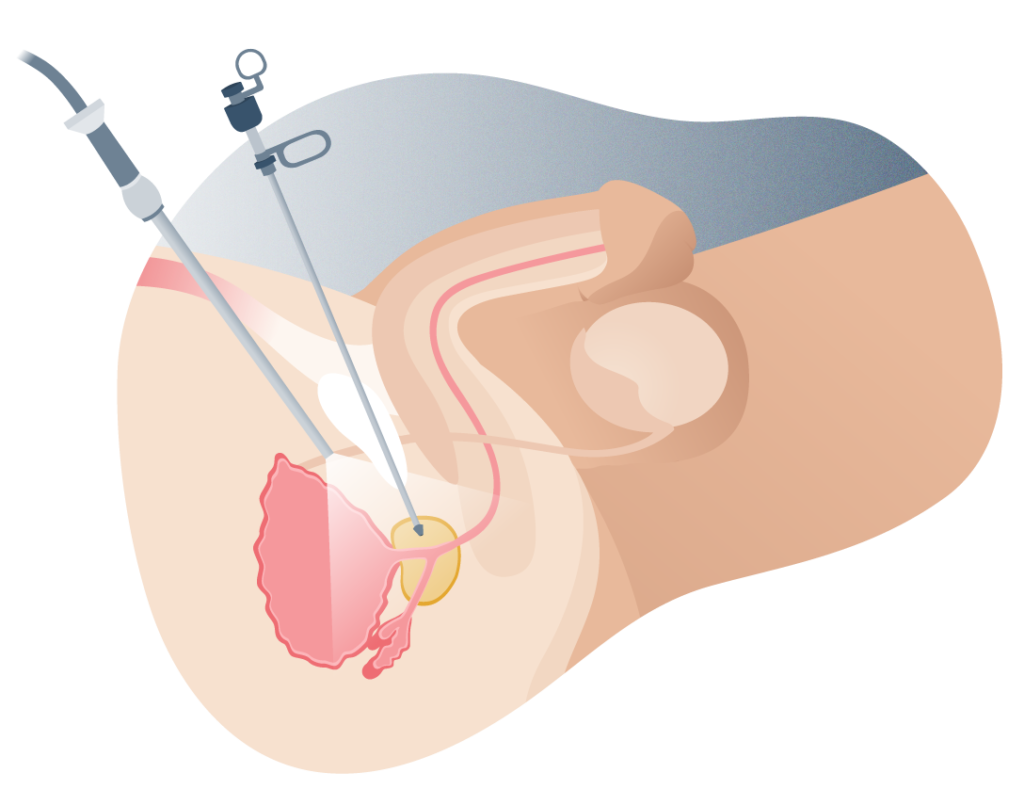
TUR trans urethral resection of the prostate
Chronic bacterial prostatitis
In this case, the patient requires a much longer administration of antibiotics, even after the symptoms have disappeared because the infection may be latent and reappear a few later. Most of the time, this period of time is around one to three months.
However, if the symptoms reappear, it is advisable to restart the administration of antibiotics and consider the possibility of changing the medication because some bacteria can become resistant to certain antibiotics.
Chronic pelvic pain syndrome
This corresponds to the most common type of prostatitis but since the cause seems to be generally uncertain, it is advisable to indicate antibiotics in the case of bacterial prostatitis together with non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or diclofenac.
It is important to note that under no circumstances should the patient self-medicate due to the risks that he could run when combining drugs that interact with each other, among others. Only a doctor can indicate and evaluate the progress of a drug treatment.
Other treatments for prostatitis
Therapeutic prostate massages
The main objective of massages of the prostate for therapeutic purposes is to gently but firmly press the prostate gland to release excess prostate secretion that may be accumulated within it due to the inflammation itself. This reduces pressure on the prostate and it can heal more quickly.
Prostate surgery
In some very rare cases (fortunately), prostate infections can produce a severe complication known as prostate abscess if they are not treated properly in time.
These abscesses are collections of purulent material (pus), bacteria, dead cells, and prostate secretion within the prostate. They are difficult to treat with antibiotics (even in patients with competent immune systems) and often require surgical removal.
Las prostatectomías
Las prostatectomías son cirugías complejas que requieren un alto nivel de precisión técnica ya que se realiza una extirpación total (o casi total) de la próstata y los tejidos que la rondan, como algunos ganglios linfáticos o las vesículas seminales si existe diseminación de células cancerígenas en esta zona, pero el gran dilema son las estructuras no implicadas en el cáncer que podrían ser lesionadas con la intervención como los nervios eréctiles.
Las prostatectomías
Las prostatectomías son cirugías complejas que requieren un alto nivel de precisión técnica ya que se realiza una extirpación total (o casi total) de la próstata y los tejidos que la rondan, como algunos ganglios linfáticos o las vesículas seminales si existe diseminación de células cancerígenas en esta zona, pero el gran dilema son las estructuras no implicadas en el cáncer que podrían ser lesionadas con la intervención como los nervios eréctiles.
La resección transuretral de la próstata consiste en:
1 Introducir el extremo libre del resectoscopio en la uretra desde la punta del pene.
2 La punta del resectoscopio se ubica a nivel de la uretra prostática y se comienza a cortar el exceso de tejido.
3 Las porciones grandes de tejido son presionadas con pinzas especiales en el resectoscopio y se halan hacia afuera. Si son muy pequeñas, pueden atravesar el esfínter de la vejiga y quedarse ahí hasta que el paciente las orine.
4 El cirujano urólogo retirará el resectoscopio y se introducirá una sonda vesical durante algunos días (generalmente menos de 48 horas).
Signs and symptoms
Causes of prostatitis
In the vast majority of cases, prostatitis does not have a definite cause or it is not discovered and the patient feels calm because it disappears on its own. Many pains in the pelvis originate when the muscles in this region become inflamed (contractures) and compress the myriad nerves that run through this area.
Infections are less common causes of pain in the male pelvis, but they can occur and should be ruled out.
Infectious prostatitis are usually caused by bacteria that, being the usual flora of urine and feces (such as E. coli), become opportunistic pathogens in the mucosa of the urethra, crossing the tissue until they lodge in an ideal gland to reproduce: the prostate. Prostatitis is not considered a sexually transmitted disease but sexual abstinence is also recommended until the infection has passed.
Non-bacterial prostatitis is often triggered by nerve inflammation, muscle spasms, stress tension, and even previous urinary tract infections that were not treated properly, even though urine and prostatic fluid are free from laboratory tests. of pathogens.
What are the least likely causes of prostate inflammation?
Pelvic pain in men and inflammation of the prostate can also be due to some less frequent causes such as:
- Kidney stones trapped in the prostate segment of the urethra.
- Stenosis of the urethra (from various causes, but most often from scar tissue).
- Irritation and compression of the prostate after imaging studies such as cystograms.
- Muscle spasms in the pelvic floor: occurs from spending a lot of time sitting on hard or very cold surfaces, cycling without sports garments with crotch protection, sports injuries, among others.
- Benign prostatic hyperplasia (BPH), something very common in men over 50 years of age.
- Prostate cancer, in the worst case.
Próstata sana
Próstata con inflamación
"The symptoms of acute bacterial prostatitis are quite sudden and come on very intensely without warning. This leads many patients to seek medical attention immediately".
Causes
Risk factors
Almost all cases of prostatitis have unknown causes and are even usually treated (or disappear on their own) before finding the source of the problem.
However, among the main risk factors involved in the appearance of prostatitis are:
What are the stages of prostate cancer?
The system used by urologists to classify malignant prostate tumours is known as TNM and takes into consideration the status of the tumour itself (its size, location, whether there are several tumours or just one), the status of the lymph nodes in the groin area and whether or not there is metastasis.
- A urinary catheter such as the one placed when the patient has benign prostatic hyperplasia. ties or when it has just come out of a surgical intervention.
- Infections in the lower urinary tract or bladder.
- The erosion produced by kidney stones when they “go down the urethra” and are compressed in the prostate segment.
- Any urinary tract problems (including gonorrhea infections).

Pruebas de imagen (urografía y ecografía pélvica)
Las pruebas de imagen permiten evaluar de manera más precisa la obstrucción de la uretra prostática. Las principales pruebas son la urografía y la ecografía.
La urografía consiste en inyectar una sustancia que, una vez filtrada por los riñones y dispersada en la orina, se pueden realizar radiografías especiales para poner en evidencia el contorno de la vejiga y la uretra. El sitio de estrechez uretral se ubica fácilmente.
La ecografía es una prueba rápida y económica que consiste en un aparato que crea imágenes bidimensionales de las estructuras internas como la vejiga (que debe estar llena de orina) al emitir ondas de ultrasonido. Es completamente indoloro y no se emite radiación ionizante (como es el caso de la urografía).

Como se diagnostica
Diagnosis of prostatitis
Although any doctor can suspect a prostatic inflammation (not necessarily prostatitis), a urology specialist is the indicated professional to carry out the corresponding studies and diagnose the problem through the following tools:
Medical interview: What could the doctor ask me?
The doctor will ask a series of questions about the condition and will listen carefully to how the patient reports the appearance of the problem and to what extent it has affected her quality of life.
In addition to inquiring about the age and health history of the patient, some of the questions that are most often asked in the diagnosis of prostatitis are:
- When did you start to notice the symptoms?
- Have you taken any medicine for urinary discomfort? How is your sex life? Do you use protection?
- Have you experienced similar symptoms before?
- Have you suffered from urinary infections in the past?
- Do you practice any sport? Have you received a blow to the genital region?
Physical exploration
The main and fastest test to check the size of the prostate is the digital rectal examination, which consists of inserting a gloved and lubricated finger through the patient’s anus to touch the prostate.
If it is enlarged, more tests are done. Contrary to popular belief, the digital rectal examination is not painful and only lasts a few seconds.
Ultrasound
Transrectal ultrasound is a fairly effective, fast, and inexpensive imaging study to more accurately examine the dimensions of the prostate and assess whether or not it is enlarged. Ultrasound uses sound waves to create a computerized image of the organ.

Urine and fluid analysis of the prostate
Urine and prostatic fluid can be easily removed and sent to a specialized laboratory for bacteriological cultures. If there is any active or latent infectious process, it will show up in the studies and this will help determine the correct treatment (not all antibiotics are effective against all types of bacteria).
Prostatic fluid (expressed prostatic excretion or EPE) is extracted by massaging the prostate, this will release a viscous fluid through the penile urethra that will be collected in a jar.
Urine can contain not only the bacteria in question but also white blood cells or leukocytes, which could indicate an active infectious process (these cells should not be present in the urine under normal conditions).
In addition, it is possible to perform a blood test to determine the levels of prostate specific antigen, a substance that rises when there are neoplastic processes in the gland but when there is an infection, this substance can rise creating a “cancer false alarm”.
Cystoscopy
A cystoscope is a special instrument that can be inserted through the urethra to take pictures of the urinary tract and bladder. The urologist can examine the condition of the lower urinary tract with this device.
Urinary flow test or urodynamics
When the obstruction in the flow of urine is very severe, it is possible to perform a test of this type that helps to measure the force of the passage of urine through the urethra until the exact point of the blockage is found.
In most cases, lower urinary obstructions occur in the prostate (from prostatitis, BPH, or cancer), in the urethra, or in the pelvic floor muscles.
Frequently asked questions
Frequently asked questions at the Andromedi centres in Madrid, Seville and Tenerife
If prostatitis does not have an infectious cause, the prostate may heal on its own and inflammation may decrease after a few days or weeks even without treatment (although anti-inflammatories can be helpful).
In fact, bacterial prostatitis can also heal on its own without any problems (but antibiotics are recommended). However, some patients with infectious prostatitis caused by bacteria and poor immune responses may develop prostate abscesses.
These abscesses are life threatening if the infection spreads to other organs of the body, such as meningitis (infection of the lining of the brain and bone marrow). In any case, it is better to be safe than sorry by going to the doctor and requesting appropriate treatment.
If prostatitis does not have an infectious cause, the prostate may heal on its own and inflammation may decrease after a few days or weeks even without treatment (although anti-inflammatories can be helpful).
In fact, bacterial prostatitis can also heal on its own without any problems (but antibiotics are recommended). However, some patients with infectious prostatitis caused by bacteria and poor immune responses may develop prostate abscesses.
These abscesses are life threatening if the infection spreads to other organs of the body, such as meningitis (infection of the lining of the brain and bone marrow). In any case, it is better to be safe than sorry by going to the doctor and requesting appropriate treatment.
Yes, prostatitis can be prevented with certain healthy habits not only for urinary function but for the entire body such as:
• Eat foods high in vitamins and myGenerally, vegetables are ideal.
• Consume at least 8 glasses of water a day.
• Exercise or play sports regularly.
• Avoid as much as possible injuries or bruises in the genital area.
• Maintain an active but responsible sex life.
• Maintain low levels of stress and anxiety.
• Go to the urologist at least once a year after age 40 for routine check-ups.
• In the event of any urinary symptoms, see the urologist.
• Avoid self-medication.
Yes, because they help drain excess prostate secretion that may have been trapped in the glandular canaliculi during inflammation. These massages should only be performed by a specialist.
Not only are home remedies not scientifically proven, but they can also be dangerous. The Internet abounds with "magic solutions" and "home remedies" for prostatitis and other urological diseases, but these could be risky and even potentially fatal. The ideal is to go to a professional in the urological area.
Yes, prostatitis is not a contraindication to having sex. However, if the condition is very severe, it is advisable to avoid sexual intercourse until the problem is treated.
There is not enough evidence to verify this hypothesis, but everything indicates that it is very unlikely.
No, and in fact, you may need to keep taking antibiotics (and anti-inflammatories) even several days or weeks after you last had symptoms.
It depends on the case. If the prostatitis is very severe, the ideal is to take a few days off and even receive treatment in a hospital. But generally prostatitis have a good prognosis and the patient can continue with their daily activities while fully complying with the treatment.
Yes, but it is rare. This type of non-infectious prostatitis can occur from sexual practices such as very intensive prostate massages. It is important to remember that excessive manipulation of the prostate gland can inflame it and that this organ has innumerable nerve endings that can be manually stimulated, bringing sexual pleasure.
MEDICAL REFERENCES AND BIBLIOGRAPHY
- PROSTATITIS COLUMBIA UNIVERSITY DEPARTMENT OF UROLOGY
- PROSTATITIS JAMA Network
- PROSTATITIS (MALE PELVIC PAIN) UNIVERSITY OF CALIFORNIA
- GUIDELINES IN UROLOGICAL INFECTIONS EUROPEAN ASSOCIATION OF UROLOGY
- ACUTE BACTERIAL PROSTATITIS: DIAGNOSIS AND MANAGEMENT AMERICAN FAMILY PHYSICIAN
- PROSTATITIS (in Spanish) MSD MANUAL
Author
Andromedi pertenece a las organizciones médicas más destacadas en el sector de la Uro-Andrología