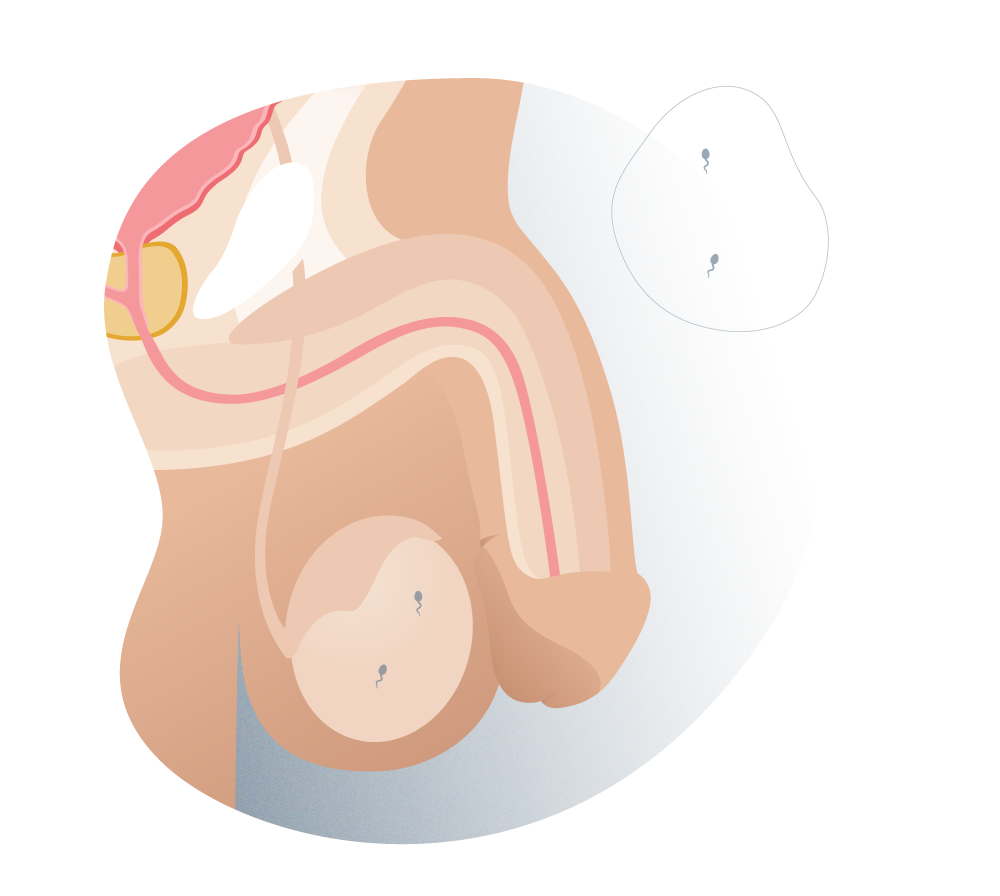
1 Normal.
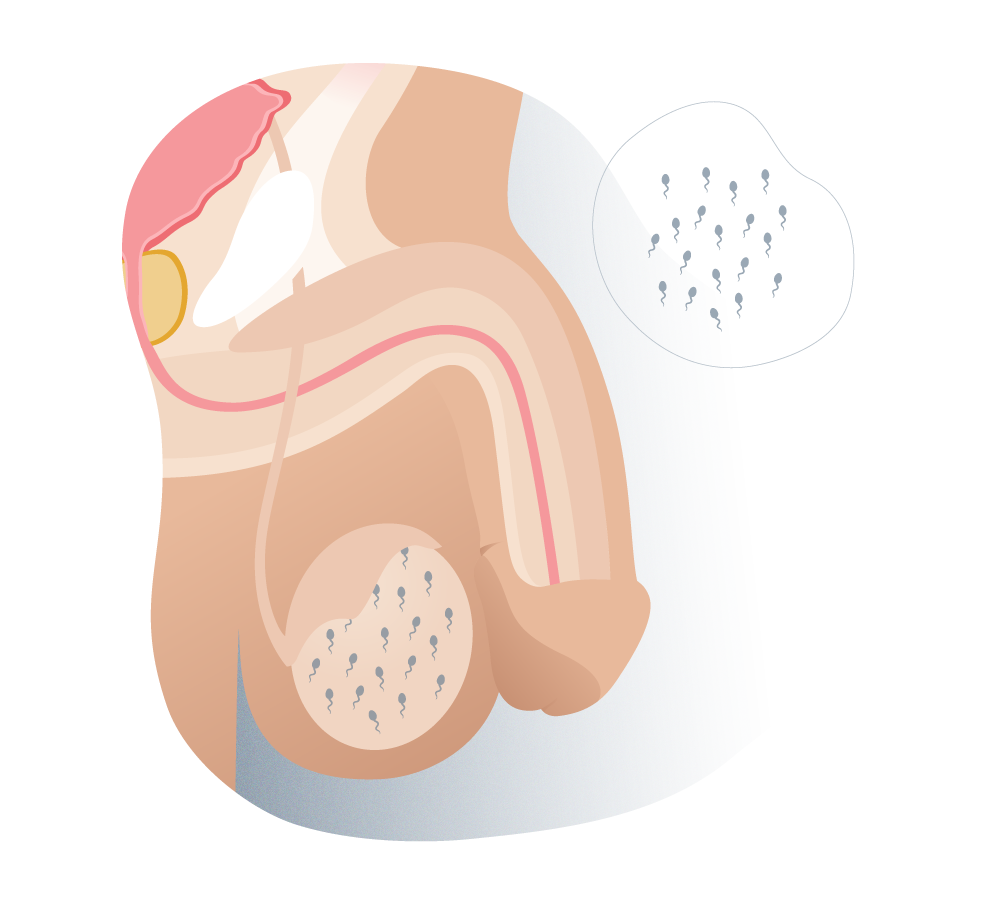
Types of azoospermia (normal)
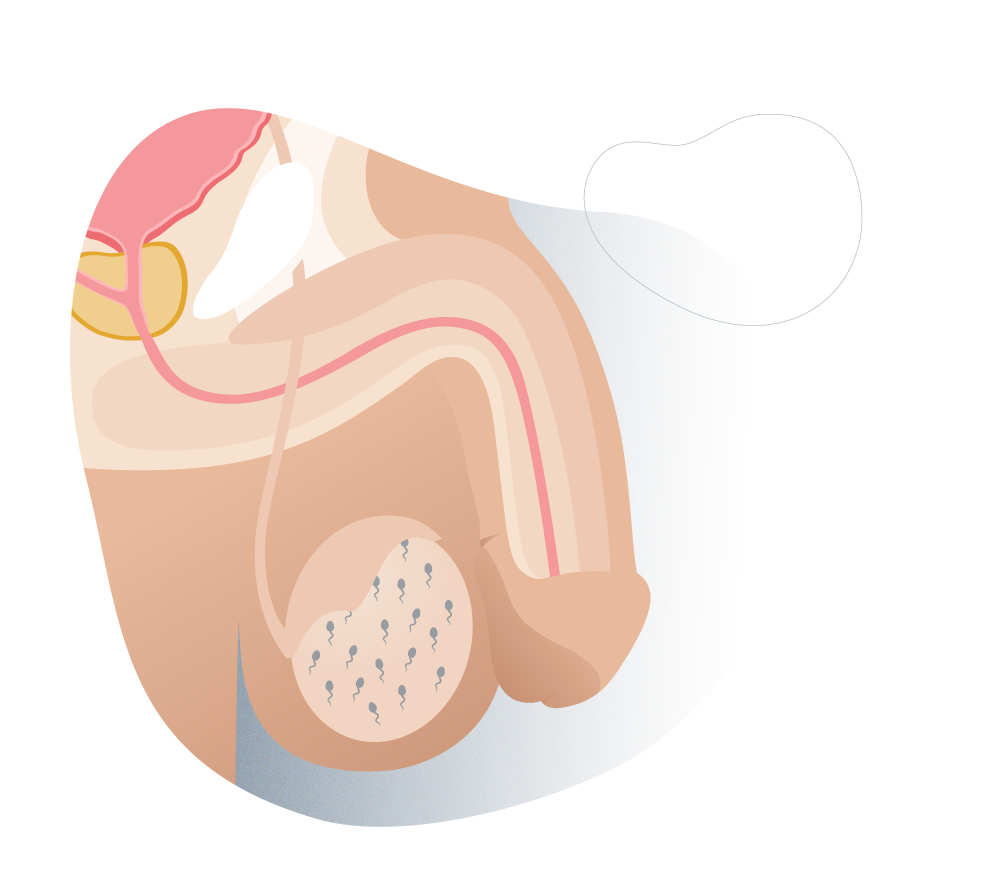
2 Pre-testicular azoospermia.
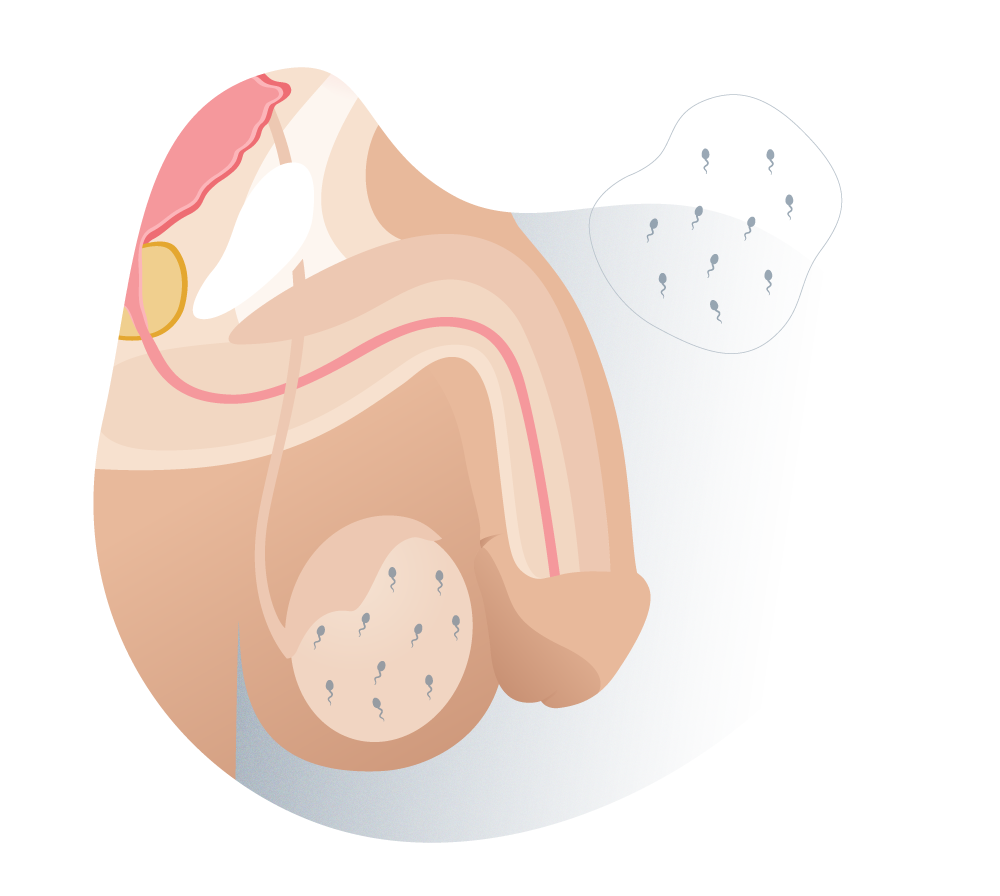
Types of azoospermia (pre-testicular)
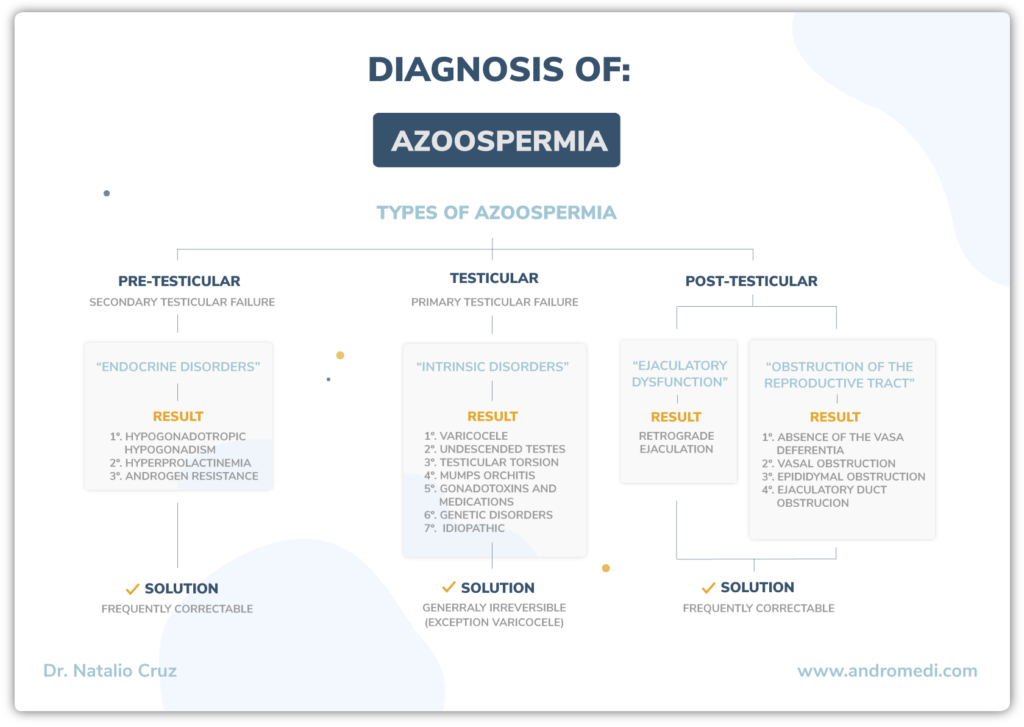
The WHO (World Health Organization) defined azoospermia as the absence of sperm in the semen or ejaculate.
The WHO (World Health Organization) defined azoospermia as the absence of sperm in the semen or ejaculate. This diagnosis should be based on at least two semen samples with a gap between them of about 4 weeks.
Info
Use our virtual assistant and receive in your email everything related to the treatments that interest you. Budgets, recovery times, hospitalization, financing possibilities month by month, etc.
In just a few minutes and without any commitment.
En cumplimiento del Reglamento General de Protección de Datos le informamos que los datos por Vd. proporcionados serán objeto de tratamiento por parte de Andromedi con la finalidad de prestarle el servicio solicitado y/o contratado. Los datos no se cederán a terceros salvo en los casos en que exista una obligación legal. Para más información puede consultarla pinchando aquí.
In practice, we distinguish two types of azoospermia: obstructive, in which sperm do not appear in the ejaculate due to an obstruction of the seminal duct, and non-obstructive, in which no sperm are produced in the testis, either due to a lack of hormones, or because of a congenital or acquired condition.
1 Normal.
Types of azoospermia (normal)
2 Pre-testicular azoospermia.
Types of azoospermia (pre-testicular)
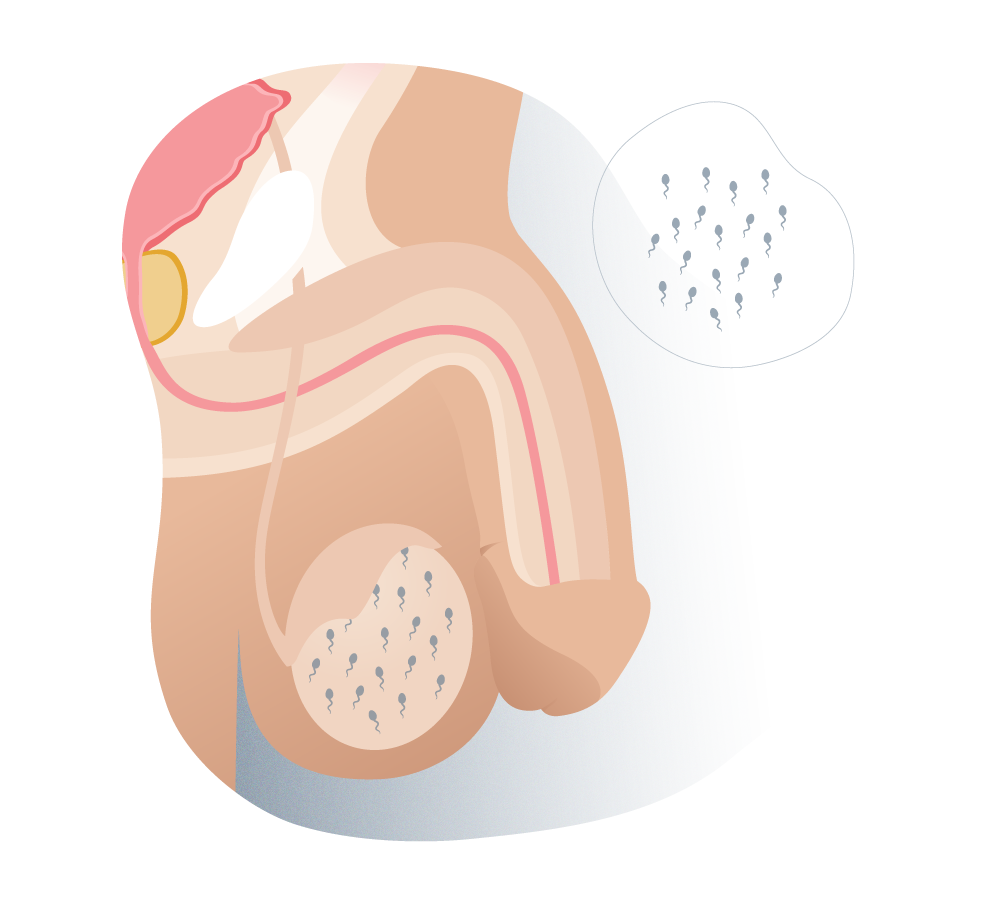
3 Testicular azoospermia.
Types of azoospermia (testicular)
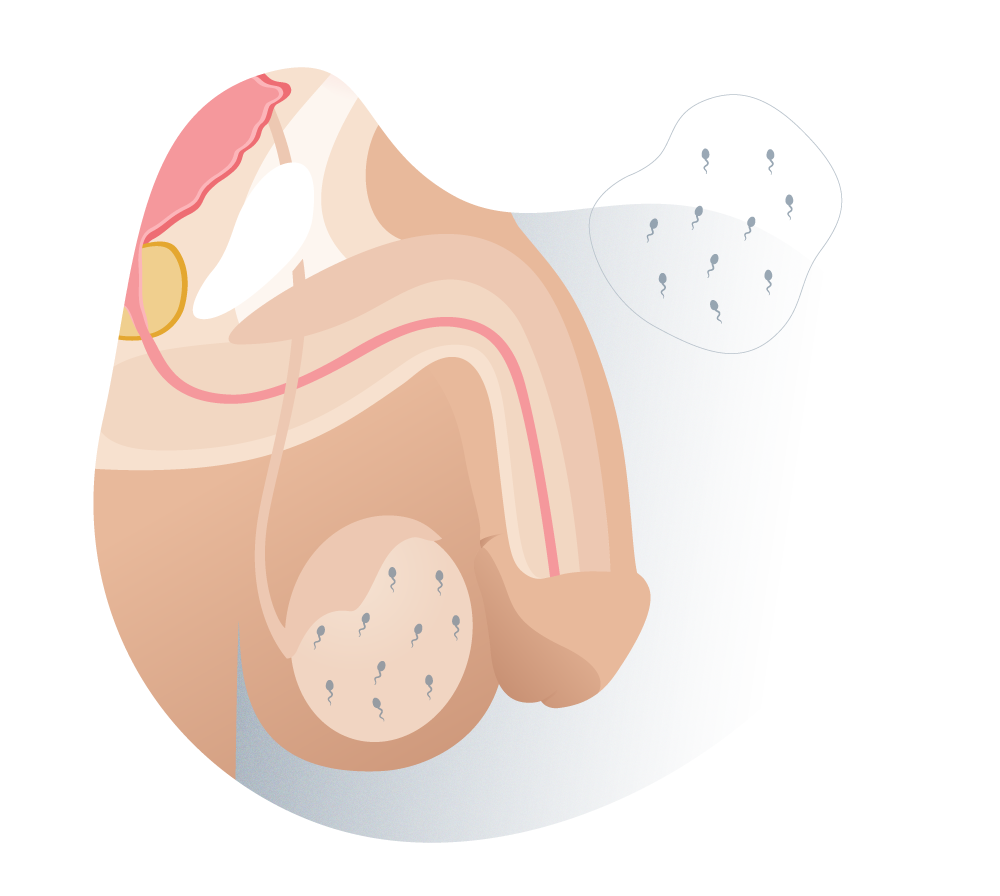
4 Obstructive azoospermia.
Types of azoospermia (ostructive)
This is short summary of the whole process: from the appointment request, to receiving the medical discharge after the treatment in some our Andromedi centers in Madrid, Seville or Canary islands (Tenerife)
Several. At least one for a medical interview and physical examination plus some genetic and laboratory tests to confirm the diagnosis.
Treatment depends on the patient's assessment and levels of a hormone called FSH. Hormone therapy shows good results.
Patients often seek help many years after the onset of the problem and this complicates treatment. Seeking help early is critical.
Treating male infertility is complicated and can take several years, but early detection is helpful.
Sex life in these patients is usually normal. This normal life depends on the patient's approach.
To keep attending medical checkups is ideal to assess the progress of treatment and sperm levels in semen.
The minimum initial evaluation should include a complete medical history, physical examination and hormonal profile, including at least FSH and testosterone in blood. Genetic testing may be of interest and recommended in some cases (suspected Cystic Fibrosis, karyotype, microdeletions of the Y chromosome, etc.).
This protocol will depend on the initial assessment and FSH levels. Hormonal treatment can be included to stimulate sperm production or a testicular biopsy may be carried out.
Remember to visit us at our Andromedi centres in Madrid, Seville or Tenerife for more information.
If it is necessary, a testicular biopsy can be performed to obtain testicular sperm. Although there are different methods, currently the most used are TESE and microTESE. Both are usually performed under local anesthesia, but can be performed with sedation if necessary depending on the case, and on an outpatient basis (no need to be admitted to the clinic)
In borderline cases, in which sperm retrieval by biopsy is believed to be virtually impossible, or in cases where conventional biopsy or TESE failed in previous attempts, the MICRO-TESE can offer an additional percentage of successful sperm retrieval. According to some authors, the success rate increases from 45 to 65% with this technique, in which a search with surgical microscope is employed.

Author
Natalio Cruz MD, with 25 years of medical experience, has been until 2016 Head of the Andrology Unit in the Urology Service of the Virgen del Rocío Hospital in Seville, National Coordinator of Andrology in the Spanish Association of Urology (AEU) and General Secretary in the ESSM, positions that he has narrowed to focus squarely on this exciting project of offering a high-level private medical consultation in Marbella, Seville, Madrid and Tenerife.
Al hacer click en “comenzar” usted declara haber leído y aceptado nuestras políticas de privacidad. El responsable de los datos que introduzcas es la Clínica Andromedi, sin cederlo nunca a terceros. El envío de comunicación privada, así como de newsletters es la finalidad de su almacenamiento en la base de datos de andromedi.com (UE). En cualquier momento puede limitar, recuperar y borrar su información, entérese cómo aquí.
Andromedi pertenece a las organizciones médicas más destacadas en el sector de la Uro-Andrología