Treatment for prostate problems
Benign prostatic hiperplasia (BPH)
Half of all men over 50 years of age have some degree of prostate enlargement that interferes with normal urinary function and causes discomfort that can put the kidneys at risk in the long term. An enlarged prostate can significantly interfere with the quality of life of any patient. The myths and taboos that surround urological check-ups do nothing more than hinder the work of doctors and delay the treatment that, generally, if applied appropriately, tends to reduce the enlargement and improve the prognosis of the disease significantly.
- VIDEO: Prostate causes erection and ejaculation problems
Benign prostatic hiperplasia (BPH)
Table of content
- VIDEO: Prostate causes erection and ejaculation problems
What is BPH
Introduction to the problems of BPH
The prostate is a male gland with sexual and urinary functions. It is located below the urinary bladder, surrounding the urethra and near the base of the penis but not inside it.
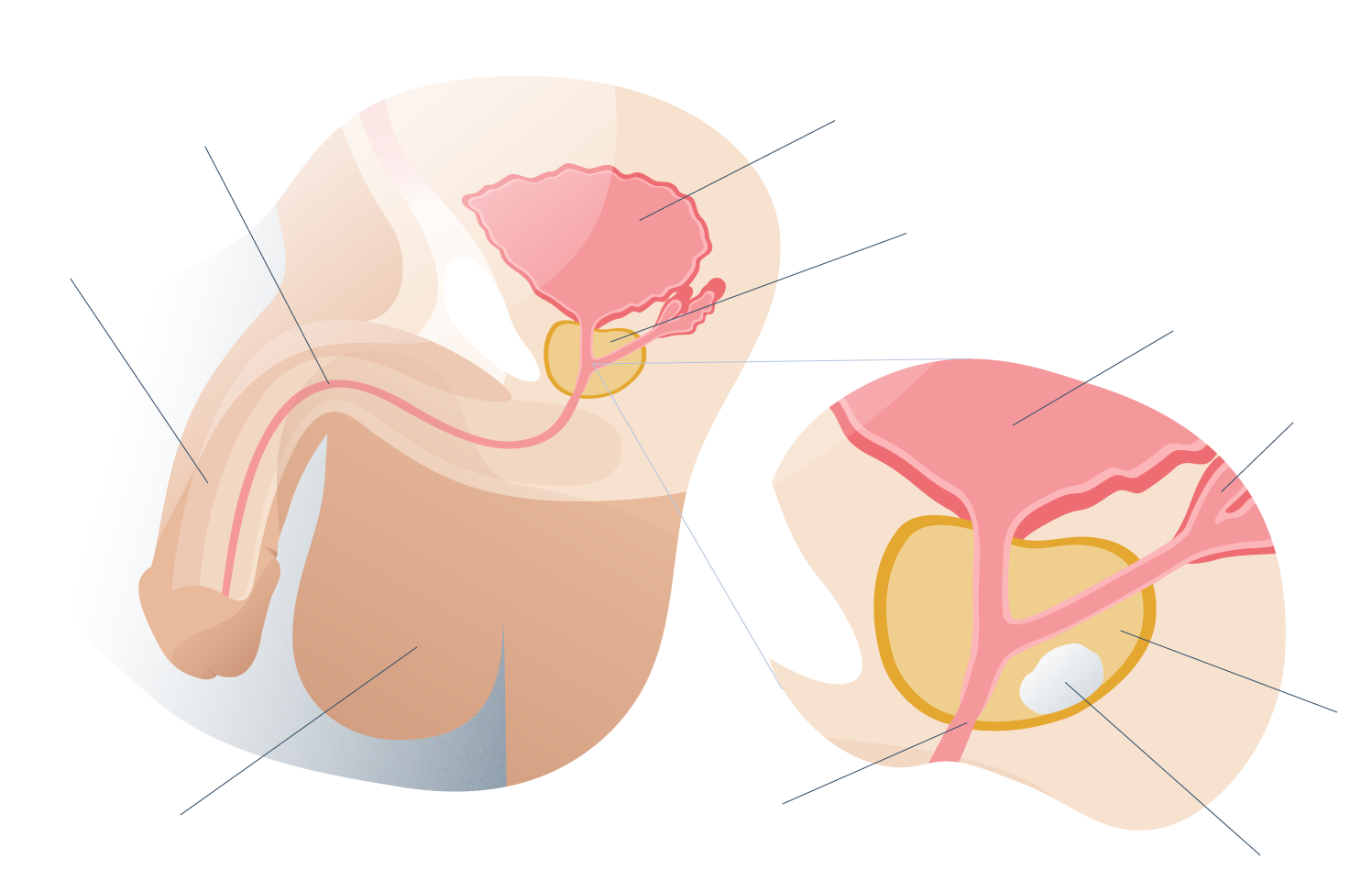
Prostate general anatomy
This gland is usually the size of a medium walnut (about 20 cc) but it tends to become abnormally large under certain factors such as age, genetic predisposition, obesity, a history of diabetes mellitus, smoking, but mainly due to the lack of the hormone most important male: testosterone.
If the levels of testosterone (and other male hormones) begin to decline progressively (as happens after the fourth decade of life) the cells of the glandular portion of the prostate swell due to the increase in androgen receptors. That is, the cells are sensitized to the little circulating hormone and therefore the gland increases its volume.
Cell growth leads to enlargement of the gland and therefore not only is it so difficult to control prostatic hyperplasia, but surgery is often necessary.
Although the normal size of the prostate is 20 cc, in some men with benign prostatic hyperplasia (BPH) glands of up to 100 cc, about five times their normal size, have been found. This can lead to urine retention and a serious urethral stricture that must be treated as a urological emergency.
The medical specialty in charge of managing cases of prostatic hyperplasia is urology and urological surgery, especially in the most severe cases where it is necessary to intervene surgically on the gland. This is a procedure known as a prostatectomy and it has many variants.
Looking for prices and information?
Use our virtual assistant and receive in your email everything related to the treatments that interest you. Budgets, recovery times, hospitalization, financing possibilities month by month, etc.
In just a few minutes and without any commitment.
En cumplimiento del Reglamento General de Protección de Datos le informamos que los datos por Vd. proporcionados serán objeto de tratamiento por parte de Andromedi con la finalidad de prestarle el servicio solicitado y/o contratado. Los datos no se cederán a terceros salvo en los casos en que exista una obligación legal. Para más información puede consultarla pinchando aquí.

PROCEDURE
Treatment of BPH

Benign prostatic hyperplasia (BPH) is a chronic disease that develops slowly and progressively and also has multiple factors associated with its appearance.
This is the reason why each case must be carefully evaluated in order to find the ideal medical treatment.
Pharmacotherapy
If the obstruction of the urinary flow due to benign prostatic hyperplasia is partial and there are only mildly bothersome symptoms (such as decreased force of the urine stream, greater effort to urinate, etc.), the pharmacological treatment that should begin with the interruption of the urine is indicated. the administration of certain medications such as:
- Anticholinergic drugs that help some patients with heart failure, asthma or constipation can complicate the obstructive signs of BPH.
- Sympathomimetic drugs, especially those with respiratory effects (to treat asthma) can also complicate the condition of patients with benign prostatic hyperplasia.
- Opioids such as codeine and other pain relievers (or drugs of abuse such as heroin) have a worse prognosis for BPH.
All of these medications increase the risk of total urinary obstruction and should only be administered carefully and if their use is really essential. After this, the treating physician may prescribe other drugs for BPH itself.
Among the drugs used as non-surgical therapy for benign prostatic hyperplasia with moderate and severe obstructive signs of the lower urinary tract are:
- Alpha adrenergic blockers such as tamsulosin, alfuzosin and terazosin that act by relaxing the smooth muscles of the urinary ducts and reducing the obstruction of the urethra.
- Treatment with alpha 5 reductase inhibitors such as finasteride or dutasteride, which act by limiting the conversion of testosterone to dihydrotestosterone, a male hormonal substance with a high capacity to produce benign prostatic hyperplasia.
Of both types of drugs, the latter have a better level of efficacy in terms of reducing the volume of the prostate and reducing obstructive signs of the lower urinary tract, especially in large prostate glands (more than 30 cc). However, excellent results have been seen combining both groups of drugs.
In cases of benign prostatic hyperplasia associated with erectile dysfunction (ED), the erection-retarding agent known as drilling afilo (or Cialis®) administered in small daily doses appears to have positive effects on obstructive and erectile disorders.
All these pharmacological treatments must be indicated by a doctor, together with periodic check-ups. Under no circumstances should the patient self-medicate.
Surgical treatment
Prostate surgery is indicated in those patients in whom drug therapy did not work or who developed complications (urinary tract infections, kidney stones, kidney damage due to hydronephrosis, etc.).
Prostate glands with volumes greater than 75 cc must be operated with open surgery due to the great risk of bleeding, infections or nerve damage.
When talking about prostate surgery, it is very likely that he is referring to the most traditional technique of operating this male gland: transurethral resection of the prostate (RTP), the standard method that, although it has undergone some changes and improvements, is still essentially the same procedure.
Transurethral resection of the prostate
Better known by its acronym RTP, transurethral resection of the prostate is a surgical technique that consists of the removal of the hyperplastic tissues of this gland by means of an endoscopic device called a resectoscope.
This resectoscope is a complex medical device that consists of an endoscope camera and a metal tip that cuts and seals tissue with thermal energy. It also has an irrigation channel that injects physiological solution to distend the urethra and improve vision.
The thin end of the device is inserted through the urethra of the penis and therefore it is not necessary to make incisions in the skin. Depending on the technology, transurethral resection of the prostate may require local anesthesia and nerve sedation or general anesthesia.
Prostate surgeries (especially RTP) can accidentally cut some nerves in the penis so that about 10% of patients may develop some sexual complication such as erectile dysfunction, or a urinary tract complication such as retrograde ejaculation or urinary incontinence.
Prostate photovaporisation with green laser
This minimally invasive technique consists of removing excess prostate tissue with an instrument that emits steam in a very precise and localized way. This reduces the risk of injuring the nerves of the penis and producing erectile dysfunction (among other possible risks of conventional surgery).
The main advantages of this technique is that the bleeding is usually minimal and the recovery is quite fast, in about 2 or 3 days the patient can return to their daily activities in a normal way.
Holmium laser prostate enucleation
Holmium laser prostatectomy (as prostate surgery is also known) is a minimally invasive technique that uses heat energy emitted by an ultra-precise laser to remove excess prostate tissue that may be blocking the flow of urine.
Holmium laser enucleation of the prostate (HoELP) can be performed transurethrally. Like the previous ones, it does not require open surgery aftercare and patients usually have a quick recovery.
"Our years of experience in the Andromedi centres in Seville, Madrid and Tenerife have shown that the combination of both drugs in a personalised way is the best strategy".
REZUM™ Technique
One of the most innovative techniques to reduce prostate volume in cases of BPH is the REZUM ™ Technique, which consists of destroying excess tissue by means of highly localized injections of thermal energy in the form of water vapor.
But if the tissue is not removed, what happens to the heat-destroyed tissue? It is important to highlight the incredible ability of the body’s immune cells to reabsorb dead tissue, as happens after the application of water vapor at high temperature. The body will only remove localized dead tissue, not nerves or healthy portions of the gland.
Since the destruction of the tissue is carried out in a controlled manner, the possibility of damaging the nerves of the penis (located outside the prostate gland) is very low compared to other surgical treatments such as transurethral resection of the prostate, laser surgery holmium or open surgery. For this reason, the REZUM ™ system has a minimal risk of complications such as erectile dysfunction or urinary incontinence.
Why is the REZUM ™ Technique so recommended?
In our clinic we have this technique and we have been able to observe surprising results: 95% of the patients experience a notable improvement in terms of the reduction of obstructive signs of the urinary tract 6 months after treatment.
Among the main advantages of this procedure are:
- Minimally invasive technique. Prostate surgery with the REZUM ™ system causes minimal impact on the body's tissues, so recovery is usually very fast and with no side effects.
- Quick procedure. Unlike golds tip In prostate surgery, this outpatient medical procedure is performed in less than 10 minutes but with surprising and long-lasting results.
- No pain or general anesthesia. The patient receives a dose of local anesthesia and some nerve sedation to be calm during surgery but not asleep (as in general surgery).
- No scars. Since the REZUM ™ technique does not require the incisions of open surgery to operate on the prostate (everything is done through the urethra) the patient is not scarred on the skin of the pubic area.
- Without entering the operating room. The REZUM ™ technique can be performed in a conditioned doctor's office and it is not necessary to admit the patient to the operating room or connect mechanical ventilation machines.
- No more drugs. Patients experience a rapid improvement in urinary obstruction due to benign prostatic hyperplasia with which they no longer need to continue taking medications. This is especially important especially in those patients in whom drug therapy causes unwanted effects such as dizziness, low blood pressure, constipation, headache, decreased sexual desire, impotence, among others.
- Long-lasting results. Only 4% of patients undergoing the REZUM ™ technique should receive a second application after five years due to the reappearance of obstructive signs. The remaining 96% of patients forget their problems due to BPH and have a normal life.
- Preservation of erectile function. The nerves of the penis (attached to the prostate gland) are not affected by the application of heat energy inside the prostate or by localized destruction of tissue. Men can feel confident that after the intervention they will not develop erectile dysfunction.
- No hospital stay. The patient undergoing therapy with the REZUM ™ system can go home immediately after treatment. It is not necessary to be admitted to the hospital for several days (this does happen with other surgeries such as RTP).
- Quick recovery. Active patients can feel confident about returning to normal activities within a couple of days after surgery with the REZUM ™ technique. Postoperative care is usually simple, no cures or infected wounds.
And how to decide the appropriate treatment?
In the first instance, conservative or pharmacological treatment should be considered. Ideally, surgical treatment should be delayed until strictly necessary.
In addition to the important opinion of the patient, the aspects that the urologist treating BPH takes into account to choose the correct treatment depend on:
- Age of the patient. Young patients tend to be better tolerant of undergoing surgery, but men over 65 years of age also tend to benefit from prostate surgery if drugs did not reverse the hyperplasia of the gland.
- Degree of prostatic hyperplasia. Treating a prostate gland with slight signs of hyperplasia (and therefore more susceptible to being treated with medications) is not the same as treating a prostate with severe hyperplasia that could even compromise kidney function. The degree of prostatic hyperplasia (determined with imaging methods such as pelvic ultrasound) is directly proportional to the degree of urethral obstruction.
- Other pathologies associated or not associated with BPH. If the patient has heart problems, is hypertensive, obese or diabetic, prostate surgery should be avoided at all costs, only until it is completely essential. Surgeries (of any kind) can complicate the state of health in susceptible or immunosuppressed patients.
- Evolution with pharmacological treatment. If the administration of drugs improved the state of prostatic hyperplasia and the degree of obstruction in the lower urinary tract was reduced, it can be considered successful, making surgery unnecessary (which obviously has a greater degree of success in reducing prostate volume). The response to drug treatment is usually most successful in the early stages of the disease.
- Feasibility of a surgery. Before each surgical intervention (including prostate surgeries) preoperative evaluations are performed to determine if surgery is necessary, what is the correct technique and what special care should be taken into account.
In cases of urinary retention, what treatment is indicated?
Urinary retention is a urologic emergency that requires immediate decompression to reduce pressure in the upper urinary tract and mitigate the potential damage to kidney tissues.
This decompression is initially achieved by introducing a standard urinary catheter into the bladder, which drains the volume of urine it contains.
If the urethral obstruction caused by hip Benign prostatic erplasia is very severe and the urinary catheter cannot cross the prostate segment of the urethra, the urologist must perform an emergency procedure known as suprapubic percutaneous decompression of the bladder, which consists of inserting a cannula from the skin of the pubis to the bladder.
These cases are rare but can occur, especially in those patients with untreated benign prostatic hyperplasia or who experienced a rapid and inadvertent enlargement of the gland due to hormonal factors.
Summary of treatment
Benign prostatic hiperplasia (BPH). What is it?
It is a urological disease of man that is characterized by an increase in the volume of the prostate gland that produces urinary symptoms. Remember to visit us at our Andromedi centres in Madrid, Seville or Tenerife for more information.
Why is it produced?
It occurs when the cells of the prostate are enlarged due to the decrease in testosterone, mainly in men over 50 years of age where half of them have BPH.
How is it diagnosed?
By means of a physical examination (digital rectal examination, anamnesis) and with imaging tests such as urethrography and ecosonogram. Blood and urine tests are also helpful.
Treatment of HBP
In the initial stages, pharmacological treatment with drugs that reduce prostate enlargement but in the advanced stages of the disease (when there is urinary obstruction) it is necessary to perform a cir surgery.
Symptoms of BPH
The main symptoms are difficulty starting to urinate, sudden feeling of wanting to urinate, urinary incontinence, going to the bathroom many times (even at night), urinary infections and bladder stones.
Surgery of HBP
Prostate surgery involves removing a portion of the gland using a device called a resectoscope in a procedure known as a transurethral resection, without incisions. More modern techniques like the REZUM ™ system have better results and it takes less than 10 minutes.
Surgical procedure
Surgery for benign prostatic hyperplasia (BPH)
The standard surgical procedure to treat benign prostate hyperplasia is transurethral resection of the prostate (or TUR), so this section will address the most important aspects of this urological operation.
The duration of this procedure is 60 to 90 minutes depending on the ease of accessing the prostate and the amount of tissue to be removed. The anesthesia used is of a general type, which means that the patient will be unconscious during the surgery.
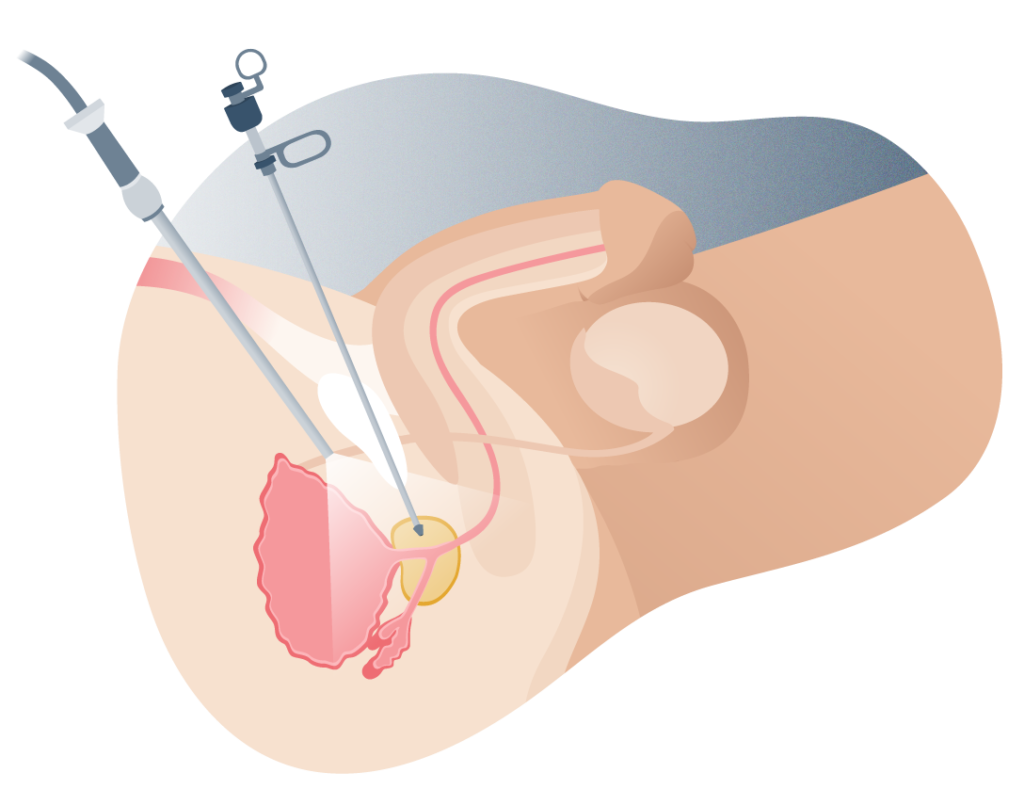
TUR trans urethral resection of the prostate
What is the goal of transurethral resection of the prostate?
As its name suggests, prostate resection (or transurethral ablation) involves removing a portion of the prostate gland through the urethra. That is, it is not necessary to make open incisions to expose the organ.
It is precisely its capacity for minimally invasive operation that makes the prognosis of benign prostatic hyperplasia so favorable and the few side effects that are usually seen with greater incidence in more conventional techniques (such as open surgery).
The device used in this procedure is known as a resectoscope and it can cut the prostate tissue through direct incisions (with a sharp tip) or with electrocautery, the most modern. This electrocautery allows not only the separation of the tissue but the immediate closure of blood vessels that may have been cut, thus reducing blood loss and the risk of infections.
This device has special forceps that allow the portion of the prostate that was cut to be taken in order to later extract it.
Procedure: What is RTP surgery?
After the patient has been initially assessed and anesthesia has been administered to avoid feeling discomfort in the urethra, the intervention proceeds.
Transurethral resection of the prostate consists of:
1 Introduce the free end of the resectoscope into the urethra from the tip of the penis.
2 The tip of the resectoscope is located at the level of the prostatic urethra and the excess tissue begins to be cut.
3 Large pieces of tissue are pressed with special forceps on the resectoscope and pulled out. If they are very small, they can pass through the bladder sphincter and stay there until the patient urinates them.
4 The urologic surgeon will remove the resectoscope and a urinary catheter will be inserted for a few days (usually less than 48 hours).
Prostatectomies
Prostatectomies are complex surgeries that require a high level of technical precision as they involve total (or almost total) removal of the prostate and surrounding tissues, such as some lymph nodes or seminal vesicles if there is spread of cancer cells in this area, but the big dilemma is the structures not involved in the cancer that could be injured with the intervention such as the erectile nerves.
Prostatectomies
Prostatectomies are complex surgeries that require a high level of technical precision as they involve total (or almost total) removal of the prostate and surrounding tissues, such as some lymph nodes or seminal vesicles if there is spread of cancer cells in this area, but the big dilemma is the structures not involved in the cancer that could be injured with the intervention such as the erectile nerves.
After prostate surgery the patient may notice certain discomforts such as irritation or burning when urinating and perhaps some blood in the urine (or very dark urine). These discomforts disappear on their own but if the patient notices any of the following symptoms, they should see a doctor:
- Inability to urinate (very painful or forced urination).
- Large amount of blood in the urine.
- Fever greater than 38 ° C (100 ° F).
Preparation for surgery
Before prostate surgery, the patient must undergo certain preoperative evaluations that consist of:
- A complete physical examination including history, digital rectal examination, check for obstructive urinary symptoms, etc.
- Blood and urine tests.
- In some cases, a urethrogram.
It is recommended that the patient, several days before surgery (it all depends on the doctor’s recommendation), stop taking certain medications such as:
- Nonsteroidal pain relievers (NSAIDs), unless absolutely necessary.
- Blood thinners such as warfarin or acetylsalicylic acid (aspirin).
If the patient has had a recent urinary infection, antibiotics may be prescribed.
Other preparations for RTP prostate surgery include:
- Organize the way the patient returns home: the ideal is to attend the clinic accompanied.
- Recovery time can vary from two to six weeks, the patient should be aware of this.
- It is recommended that the patient clean the genital area with neutral pH soap and water before surgery and shave the pubic hair.
Postoperative care and patient follow-up
Among the main recommendations for men undergoing prostate surgery are:
- Increase your fluid intake, mainly water or fruit juices (avoid highly acidic juices so as not to alter the pH of the urine).
- Consume foods with fiber to prevent intestinal constipation and decrease the effort to evacuate.
- Abstinence from alcohol, tobacco and other medications (unless the doctor ensures that they are not risky).
- Avoid physical exercise and strength activities such as heavy lifting for about five weeks.
- Avoid having sex for five weeks (or the time stipulated by the doctor).
- Avoid driving a car, at least for as long as the urinary catheter is inserted.
RTP results
After transurethral prostate resection surgery, the reduction in the volume of the prostate is instantaneous but the improvement in urine flow and the decrease in urine retention may be fully perceived within a few days after removal of the urinary catheter.
A condition with a solution
Now that we know your solution, what is HBP?
Although it seems a definitive diagnosis, benign prostatic hyperplasia is a condition that has a solution. This section will delve into the clinical picture produced by this disease that affects older men.
Why does BPH cause so many problems?
The prostate is a gland that is located around the urethra, just below the sphincter of the urinary bladder. If the prostate becomes inflamed, the tissue growth is concentric, that is, towards the urethra.
When the urethra is compressed and there is obstruction of urine, the bladder exceeds its storage capacity and incontinence (when the pressure within the bladder is so great that it passes through the site of prostatic compression in the urethra) or a kidney problem known as hydronephrosis, in the worst case.
Incomplete emptying of the bladder can predispose to urinary tract infections and kidney stones (commonly known as kidney stones).
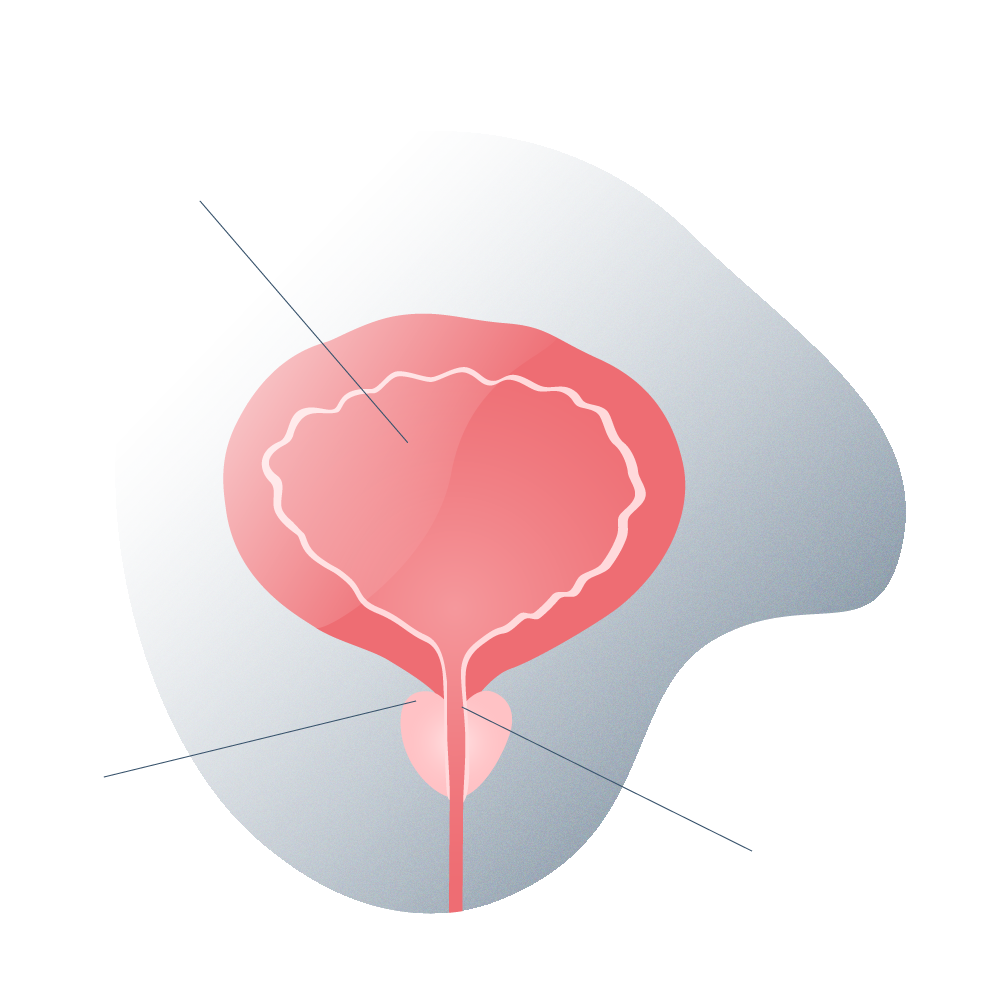
Healthy prostate
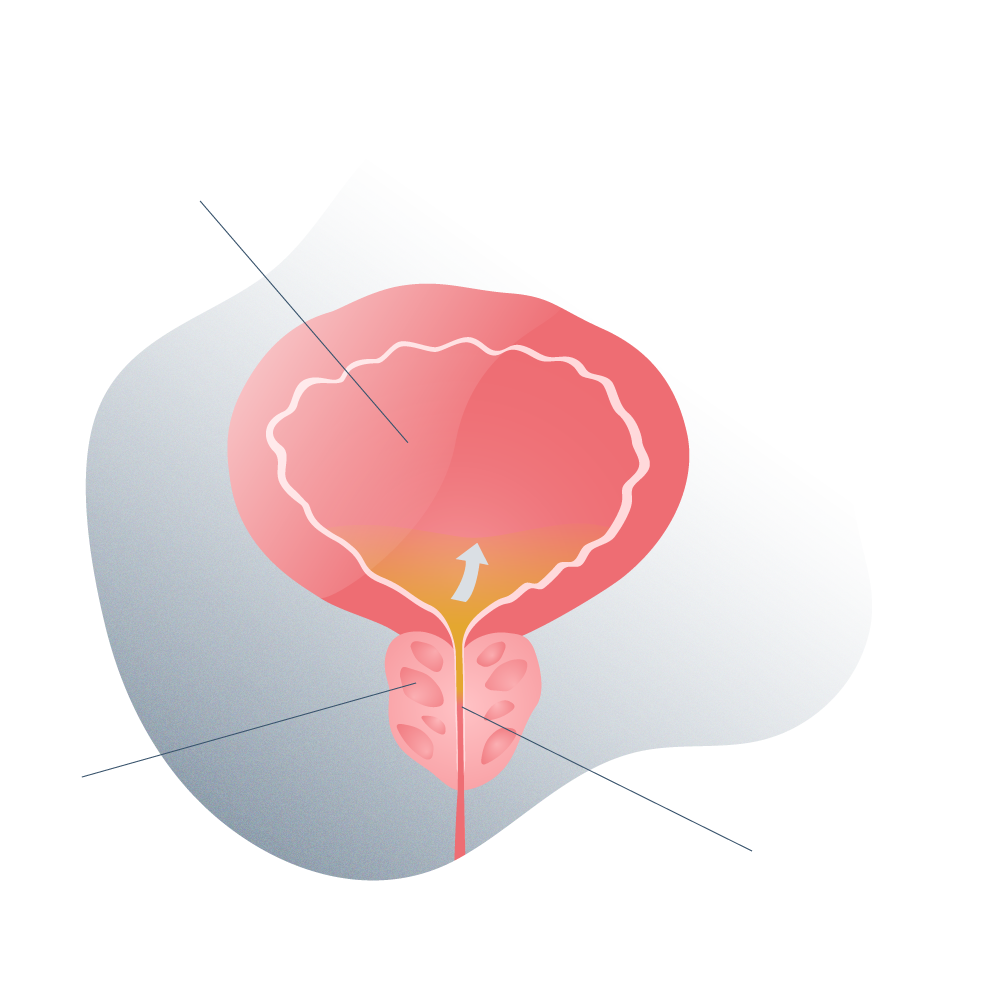
Prostate with inflammation
How common is BPH?
According to official data, about 105 million men suffer from benign prostatic hyperplasia (BPH) to some degree and perhaps many of them still do not know it. This complicates treatment since most of those affected only go to the doctor when they perceive obstructive signs in the urinary flow (indicating moderate or severe hyperplasia) and are not diagnosed in the early stages of the disease (by means of a simple check-up urological).
Benign prostatic hyperplasia (BPH) is a condition that does not develop suddenly but can take several years (even decades) to manifest clinically. Often, BPH begins at age 40, and in fact, 50% of 50-year-old men have it, and by age 80, 90% are already affected.
"Benign prostatic hyperplasia (BPH) is a condition that does not develop suddenly but can take several years (even decades) to manifest itself clinically".
Problems arising
Signs and symptoms of BPH
The symptoms of benign prostatic hyperplasia are closely related to the obstruction of the lower urinary tract itself, and of these, the most commonly reported by patients are:
- Polakyrie: or the increase in voiding frequency throughout the day. The patient goes to the bathroom several times but only manages to urinate a few drops and feels that he has not urinated completely.
- Nocturia: if the urge to urinate is very frequent at night.
- Urinary urgency: or a very strong feeling to urinate that comes on suddenly.
- Difficulty starting to urinate: perhaps the patient makes a great muscular effort with the abdomen to begin to release urine.
- Intermittent urine stream.
Only very few patients experience pain when urinating, especially in those who must compress the abdominal muscles and hold their breath to “compress” the bladder. However, if the force exerted when urinating is very great, the patient can cause aggravation of hemorrhoids, inguinal hernias or urinary bleeding due to ruptured veins in the bladder.
Prostate enlargement symptoms test
Many patients, before going to urological consultation, know that they suffer from urinary problems but do not know the seriousness of the matter. However, there is a quick and easy way to assess the degree of urinary obstruction due to benign prostatic hyperplasia through a test.
This test (called IPSS or International Prostate Symptom Score) consists of the following questions, which will be given a score ranging from 0 to 5 (0 being the lowest grade and 5, the highest grade):
1 How many times have you had to urinate again within two hours after initially urinating?
2 How often do you have to put up with the urge to urinate?
3 In the past 30 days, how often did you get out of bed to urinate at night?
4 How many times have you felt the sensation of not having completely emptied your bladder?
5 How many times have you noticed that after you started urinating you had to stop and then start urinating again?
6 How often have you observed that the urine stream has lost strength or is very weak?
7 How often do you have to squeeze your muscles? abs to start urinating?
8 How would you feel if you had to spend the rest of your life with prostate symptoms as you do now?
Each score is added to the rest and the final score is used for interpretation with the following guide:
- Mild symptoms: scores from 1 to 7.
- Moderate symptoms: scores from 8 to 19.
- Serious symptoms: scores from 20 to 35.
This questionnaire can not only be done by the patient himself but also allows the doctor to evaluate the response to treatment.
Testing and analysis
Diagnosis of BPH

The diagnosis of benign prostatic hyperplasia begins as soon as the patient talks with the doctor about his urinary symptoms and to what extent they are affecting him. This part of the diagnosis is known as anamnesis and it is where the doctor begins the collection of important data to prepare the medical history such as:
- Age of the patient.
- Occupation.
- Life habits (diet, exercise, sex life, tobacco, alcohol consumption, stress, etc.).
- Family history of BPH (father, uncles or brothers with this disease).
- Previous illnesses such as high blood pressure or diabetes mellitus.
- Urine infections.

El robor Da Vinci es última tecnología e innovación
Also, the doctor will do a physical examination and order some special tests. This physical examination is based on palpation of the outer surface of the prostate by means of a digital rectal examination.
What is a digital rectal examination?
Digital rectal examination is a quick and easy diagnostic method that involves touching the prostate to measure its size and other characteristics.
Some men have a certain taboo with this procedure, but scientific studies confirm that the digital rectal examination is one of the most useful and reliable tools to examine the prostate.
The doctor puts on latex gloves and in a matter of seconds inserts a finger through the anus to feel the posterior wall of the male gland. It is somewhat uncomfortable but not painful.
Blood test: Prostate Specific Antigen (PSA)
If the prostate gland is enlarged and has been evidenced with a rectal examination, it is important to determine the blood levels of a substance known as prostate specific antigen or PSA.
Prostate specific antigen is a protein produced by the prostate that is associated with the risk of prostate cancer.
If PSA levels are within the normal range (less than 4 ng / ml) and the prostate is enlarged, it may be benign prostatic hyperplasia. But if PSA levels are very high, it is possible that it is a malignant process in the gland. The main differential diagnosis of BPH is prostate cancer.
Urine analysis
Urine tests are used to determine the chemistry of this substance, kidney function and the presence or absence of pathogens causing infection.
Benign prostatic hyperplasia can often cause urine retention in the bladder and increase the risk of infections, especially in patients with diabetes or immune problems.


Imaging tests (urography and pelvic ultrasound)
Imaging tests allow a more precise evaluation of the obstruction of the prostatic urethra. The main tests are urography and ultrasound.
Urography consists of injecting a substance that, once filtered by the kidneys and dispersed in the urine, special X-rays can be made to reveal the contour of the bladder and urethra. The urethral stricture site is easily located.
Ultrasound is a quick and inexpensive test that consists of a device that creates two-dimensional images of internal structures such as the bladder (which must be filled with urine) by emitting ultrasound waves. It is completely painless and no ionizing radiation is emitted (as is the case with urography).

How to prepare for the urological evaluation?
Ideally, the patient attends the urological consultation with a full bladder (in case it is necessary to perform a pelvic ultrasound) and having performed proper hygiene of the genital area.
Also, it is useful that the information provided by the patient is as accurate as possible so it is advisable to note the urinary symptoms that appear, with what factors increase or decrease, if they have worsened and other relevant data on urinary function and the state of general health.
Risk Factors
What are the risk factors for BPH?
Among the most important risk factors associated with the development of benign prostatic hyperplasia are:
- Age. Clinical observations show that age is the main risk factor involved in the development of benign prostatic hyperplasia, especially in men over 50 years of age where half already have some sign of prostate enlargement that worsens over time.
- Genetics. The relationship is not yet completely clear, but observations indicate that having or having had a famil A close relationship with an enlarged prostate (father, grandparents, uncles, siblings) increases the risk of developing BPH.
- Diabetes. This metabolic disease favors not only the hyperplasia of prostate cells but also inflammatory processes throughout the body.
- Elevated levels of lipids in the blood. Dyslipidemias, as they are known, and cardiovascular diseases in general such as high blood pressure seem to have a strong relationship with prostate hyperplasia, especially in men receiving beta-blocker medication.
- Unhealthy lifestyles such as sedentary lifestyle, high calorie diets, low water and vegetable consumption, smoking, high alcohol consumption, etc.
Care
Prevention of BPH
Although genetic factors and advanced age are the main risk factors in the development of benign prostatic hyperplasia (BPH), there are certain healthy habits that, being adopted, can reduce the probability of suffering from this urological disease.
The following healthy lifestyle is not only helpful in preventing BPH but in ensuring optimal overall health in men:
- Physical exercise such as running (light walks if there is physical limitation), water sports, cycling, hiking, etc. The combination of weight lifting and cardiovascular exercise has a special positive effect on health in men over 50 years of age as it helps to maintain testosterone levels and maintain physical strength.
- Adequate water consumption to keep body tissues hydrated and prevent thrombus formation.
- A balanced diet, high in protein and vegetables, low in fat.
- Supplementation with omega 3 and oils high in good fatty acids such as olive or linseed oil.
Possible negative developments
Complications of BPH
If benign prostatic hyperplasia (BPH) is not treated properly, the following complications may develop, especially in men with previous diseases:
- Urinary tract infections (UTI) as urinary retention can promote the proliferation of bacteria in the bladder and urethra.
- Complete urinary retention, which requires inserting a urinary catheter or catheter to drain excess urine and reduce pressure within the upper urinary tract.
- Kidney stones since urinary retention favors the deposit of minerals in the urine and the formation of crystals that, if they become too large, must be removed with surgery.
- Lesions in the urinary bladder due to increased internal pressure of the organ and distension of the walls.
- Kidney injury from increased pressure in the medulla of the kidneys or from infections.
- Overflow urinary incontinence (when the bladder is so full of urine from a blocked prostate and urine comes out suddenly).
Frequently asked questions
Frequently asked questions at the Andromedi centres in Madrid, Seville and Tenerife
The anesthesia used depends directly on the type of surgical intervention. For example, in the standard procedure to operate the prostate (transurethral resection) it is necessary to administer general anesthesia but in the most modern surgical techniques such as the REZUM ™ system only require local anesthesia and some nerve sedation. The patient can remain conscious throughout the surgery (which takes about 7 minutes, in fact).
If prostatic hyperplasia is not treated properly and at the right time, the quality of life of the man can be diminished: sexual potency decreases and problems of urinary incontinence or difficulty urinating can ruin the normal development of daily activities such as going out with friends or enjoy a movie day.
The section “complications of BPH” delves into the consequences of delaying the diagnosis and treatment of this disease.
Sexual intercourse can be enjoyed normally despite an enlarged prostate if erectile function has not been affected. An active sex life is indeed beneficial in treating BPH.
If a man undergoes surgery to remove excess prostate volume, he must wait a few weeks (between two and six weeks) to have sex again. The treating doctor will indicate the appropriate time, this helps reduce the risk of bleeding and urinary infections.
Having a direct male relative with benign prostatic hyperplasia increases the risk of developing the disease. For this reason, it is advisable to perform periodic medical check-ups after a certain age (the first urological check-up should be at the m before age 40).
It depends on the case, but generally the reduction in prostate volume is such that patients can stop taking drugs for hyperplasia of the gland.
It is unlikely but it can occur, especially in men with a genetic predisposition to prostate cancer. There is still no clear relationship between the two diseases.
By itself, benign prostate hyperplasia does not cause erectile dysfunction (remembering that the nerves responsible for this function only run through the gland outside of it and are not affected by enlargement) but it is possible to develop retrograde ejaculation problems.
Retrograde ejaculation can interfere with fertile capacity and occurs when the prostate enlarged by BPH compresses the seminal ducts and forces them to transport semen to the urinary bladder (where it combines with urine) and is not ejaculated at the time of male orgasm.
The reported cases are very few but it is possible. Ideally, consult your doctor as soon as you notice signs of obstruction in the lower urinary tract (difficulty starting to urinate, intermittent, painful or multiple urination at night).
These symptoms could be part of the clinical manifestation of benign prostatic hyperplasia or other urological pathologies.
Diabetes mellitus (especially uncontrolled diabetes) can not only promote the appearance of benign prostatic hyperplasia (BPH) but also worsen the clinical picture of patients with this disease.
High blood glucose levels can promote the development of urinary infections and complicate the treatment of BPH.
Diabetic patients with benign prostatic hyperplasia should undergo periodic check-ups to assess urinary tract symptoms and also measure response to treatment.
Yes, and it occurs by storing urine for long periods within the urinary bladder. This leads to a proliferation of bacteria and invasion of tissues. In this case, urinary tract infections should be treated with specific antibiotics for the pathogen that has been identified with bacteriological cultures and other laboratory studies.
There is insufficient scientific evidence to confirm the biochemical mechanisms by which Saw Palmetto (Serenoa repens) supplements have positive effects in reducing prostate volume but apparently can help. However, it is advisable to attend with the doctor and not self-medicate.
Thousands of videos on YouTube talk about home remedies and natural therapies to "eliminate prostatic hyperplasia" but most can be dangerous to health.
The most observed side effects of this procedure are urinary bleeding (which should stop on its own after four weeks after surgery) and retrograde ejaculation, however, they are rare.
There are other even rarer side effects such as:
Erectile dysfunction due to damage to the nerves of the penis.
Chronic irritation of the urethra and burning when urinating.
Stenosis of the urethra due to tissue scar formation.
Urinary incontinence due to dilation of the bladder sphincter.
Fertility problems from retrograde ejaculation (when semen passes into the bladder instead of being expelled through the penis).
Medical references and bibliography
- International Prostate Symptom Score (IPSS) (en inglés) Medscape Web
- Prostate Enlargement (en inglés) The NHS Website
- Benign Prostate Hyperplasia (en inglés) National Institute of Diabetes and Digestive and Kidney Diseases
- Causes and Symptoms of benign Prostate Hyperplasia (en inglés) Mayo Clinic
- Benign Prostate Hyperplasia: a Urological Condition (en inglés) Saint John Cancer Hospital
- Relation between diabetes and BPH (en inglés) PubMed
- Pharmacological treatment for Benign Prostate Hyperplasia (en inglés) WebMD
- REZUM™ Technic for BPH (en inglés) NCBI - US
- Surgery for Prostate Enlargement (en inglés) WebMD
Author
Natalio Cruz MD, with 25 years of medical experience, has been until 2016 Head of the Andrology Unit in the Urology Service of the Virgen del Rocío Hospital in Seville, National Coordinator of Andrology in the Spanish Association of Urology (AEU) and General Secretary in the ESSM, positions that he has narrowed to focus squarely on this exciting project of offering a high-level private medical consultation in Marbella, Seville, Madrid and Tenerife.
Andromedi pertenece a las organizciones médicas más destacadas en el sector de la Uro-Andrología