fertility TREATMENTS
Vasectomy
Vasectomy is a permanent contraceptive method for men, it is based on the ligation of the vas deferens at the scrotal level in order to prevent the passage of sperm from the epididymis and that go to the urethra at the time of ejaculation.
- VIDEO: Vasectomy, and other fertility treatments with high success rates
Vasectomy
Índice de contenido
- VIDEO: Vasectomy, and other fertility treatments with high success rates
DEFINITION
Introduction
Vasectomy is a permanent contraceptive method for men, it is based on the ligation of the vas deferens at the scrotal level in order to prevent the passage of sperm from the epididymis and that go to the urethra at the time of ejaculation.
This minor surgery is performed in men of reproductive age as a contraceptive method that, at the same time, can be definitive, long-lasting (over time) but without ceasing to be reversible (thanks to a surgery called vasovasostomy). The level of safety offered by vasectomy is close to 100 percent, making it, in the long term, the most reliable and complete definitive male contraceptive method, since it offers total safety and is reversible.
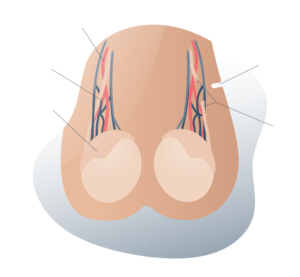
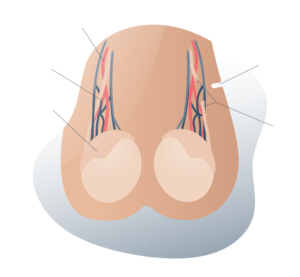
Simplified view of vasectomy
Simplified view of the vasovasostomy
Looking for prices and information?
Use our virtual assistant and receive in your email everything related to the treatments that interest you. Budgets, recovery times, hospitalization, financing possibilities month by month, etc.
In just a few minutes and without any commitment.
En cumplimiento del Reglamento General de Protección de Datos le informamos que los datos por Vd. proporcionados serán objeto de tratamiento por parte de Andromedi con la finalidad de prestarle el servicio solicitado y/o contratado. Los datos no se cederán a terceros salvo en los casos en que exista una obligación legal. Para más información puede consultarla pinchando aquí.
Medical evaluation
Why do I or not get a Vasectomy?
Reasons why I Should have a vasectomy
Opt for a vasectomy:
- If you are looking for a long-lasting and effective contraceptive method
- If you intend not to have more offspring.
- If you do not want or do not tolerate the use of latex condoms to prevent unplanned pregnancy
- If you do not want to use a condom and your partner cannot or does not want to use other contraceptive methods such as the IUD, the Ogino method, ligation, pills or the uncomfortable coitus interruptus or “reverse”. With a vesectomy, both members of the couple can feel the security and confidence of enjoying sexual intercourse without any other method to avoid fertilization.
- If you are looking for an outpatient surgical procedure, fast and that does not require the patient to be admitted to the hospital.
- For reasons of economic profitability: the economic and physical cost of a vasectomy is much lower in the long run than any other, such as that of a uterine tubal ligation surgery
- If you want it to be slightly surgically aggressive: the surgery is minimal, painless, and post-surgical recovery is simple and does not require care other than the protection of the small operative wound for a few days
- If you want a method that allows you to resume your sexual activity soon: after a vasectomy, the man can return to his usual sexual life in 24-48 hours after the intervention.
- If you want to avoid undesirable effects on your erection and orgasm: vasectomy does not cause sexual dysfunctions of any kind, nor does it leave external marks or scars that are annoying
Reasons NOT to have a vasectomy: possible downsides
Vasectomy is a method that prevents unwanted or planned pregnancies and is quite safe. However, it is vitally important that the patient knows the following implications:
- Vasectomy is a surgical contraceptive procedure, so you cannot have children naturally unless you undergo again vasectomy reversal surgery (vasovasostomy) again.
- Before vasectomy, semen can be preserved in a sperm bank (by cryopreservation in liquid nitrogen), to be used through in vitro techniques in the event that you regret it and do not want to re-operate
- Vasectomy reversal surgery (vasovasostomy) is more expensive than the vasectomy itself.
- In young men, vasectomy is not recommended. It is necessary to be 18 years old to sign the informed consent or that it is authorized by the parents or legal guardians. Generally this technique is more requested by adult men who have previously had children, although it is not a legal requirement and the desire of the male over 18 years of age prevails
- Vasectomy does not protect against sexually transmitted infections (STIs) such as HIV, HPV, genital herpes, or any other.
- Vasectomy does not affect sexual function..
But in a single man, is it possible? Makes sense?
Often the men who decide to have a vasectomy are mature adult men who have probably already had children and who are in a stable relationship. However, in recent decades it has begunthere will be a boom in young, single, childless men who voluntarily decide to be vasectomized.
Every case is different and every opinion must be respected. In our case, we will try to guide each man and help him find a suitable contraceptive solution.
The level of safety offered by vasectomy is close to 100 percent, making it, in the long term, the most reliable and complete method of definitive male contraception, as it offers total safety and is reversible.
Vasectomy Reversal
Treatment Summary
Here is a summary of the approximate process from the time you make your appointment until you are discharged from the hospital after treatment. You can receive treatment at any of our centres in Madrid, Seville or Tenerife.
Necessary Consultations
Two consultations. One to discuss the procedure with the doctor and one for the pre-operative vasectomy assessment.
Hospital Stay
When the patient's anaesthesia wears off and the doctor has checked that everything is OK, the patient can go home
Type of anaesthesia
Local but sometimes accompanied by some general sedation. In the end, there are usually no scars or marks on the scrotum.
Intervention Time
Vasectomy is a very quick procedure as it is minimally invasive. It takes about 30 to 45 minutes.
Postoperative
Complete rest the day after vasectomy and sexual abstinence for a minimum of three days is recommended
Normal Life
There are no visible scars and sex life can continue normally and the patient can feel confident in the level of security.
Techniques and treatments
Level of efficiency
When the effectiveness of this method is measured, the absence of pregnancies is evaluated, with vasectomy having a failure rate of around 0.5%.
Post-operative semen analysis is a fundamental part of evaluating the effectiveness of the surgery and for the required follow-up of the patient, this is preferably done 3 months after the vasectomy, when the patient has already had 20 to 25 ejaculations. , due to the slowness with which the sperm move in the vas deferens, which measures approximately 50 centimeters in length.
It is important to remember that as long as the seminogram does not result in the total absence of sperm, the patient must continue to use an additional contraceptive method during sexual intercourse, and the examination must be performed monthly until azoospermia is determined.
In some cases, a low number of immobile spermatozoa (less than 100,000 immobile spermatozoa per milliliter) may persist for a long period of time. In these cases, patients may also be discontinued, since many studies have shown that after 3 years azoospermia is reached.
If the seminogram shows the total absence of sperm, the operation will be considered successful and the patient will be able to have sexual intercourse without the need to use other contraceptive methods and without fear of unwanted pregnancies.
Usually 80% of men achieve these results after 3 months after surgery. In case of persistent motile sperm after 6 to 8 months of follow-up, it is advisable to redo the vasectomy.
Vasectomy Vs. other male contraceptive methods
For a long time, men contributed to birth control through intercourse interruptus, the condom, or the rhythm method, but with the advent of female contraceptives (such as the hormonal pill) or uterine tubal ligation, women began to take a key part in pregnancy planning.
However, if one is compared to the other, it is much more efficient for the male to have a comfortable, oral contraceptive method (preferably) and of course, reversible at will. And this is where the vasectomy appears.
Vasectomy has a confidence level of almost 100% if the appropriate measures are taken, plus it is natural for men because it does not interfere with sexual desire, the strength of erections, or ejaculation itself.
The intercourse interruptus or “reverse” method involves removing the erect penis from the vagina just before ejaculation, but the failure rate is already high: almost 23%. This, because the precum or precum (which is released involuntarily during sexual arousal) may contain sperm remnants.
On the other hand, the rhythm or Ogino method consists practically in completely abstaining from intercourse during the ovulatory period of the woman (a few days before and some several more, after) but in the same way, the failure rate can be up to 24% if it is not accompanied by a latex condom or the female menstrual period is regular (which is usually not as frequent as it is thought).
And finally, there is the male contraceptive method par excellence: the condom, which must be used appropriately, with only one use to avoid ruptures. The condom has proven to have good results not only in preventing unwanted pregnancies but also in preventing the spread of STIs.
Even with all this, many men (and their partners) consider it uncomfortable not only because of its use in each sexual act but also because of the allergies that it can cause in some people and the obvious decrease in skin sensitivity and its failure rate it is around 10%.
However, vasectomy is the surgical method of choice to achieve a simple, cheap, effective and definitive contraception in men. It is performed in less than 30 minutes, it is highly reliable, natural, with minimal negative effects on sexuality, and reversible through an even simpler surgery: recanalization of the vas deferens or simply vasovasostomy.
Contraceptive counseling:
Vasectomy should be considered as a semi-permanent contraceptive method, so both the individual and the couple should study and discuss the decision to perform this surgical procedure or not very well. It is recommended that the individual have his genetic desire satisfied in the moat the time you choose this contraceptive method.
There are certain considerations that the doctor should keep in mind:
- VIDEO: Vasectomy is reversible
- Although vasovasostomy is a surgery with high levels of efficacy in the recanalization of vasectomy, in the first instance, the latter should be considered as an irreversible method for the decision. Therefore, the patient must be convinced that he voluntarily abstains from reproduction, it is important that the decision is made in a situation without stress and without compulsion
- It is necessary to use other contraceptive measures until the success of the intervention is confirmed
- Discuss the vasectomy technique to be used, taking into account the advantages and disadvantages
- Talk about the existence of other contraceptive options, based on the reproductive moment of the individual and the couple
- Publicize the surgical techniques to reverse vasectomy and the possibilities of success or failure
- Obtain informed consent from the patient, in writing.
- Inform the patient that recanalization of the vas deferens occurs very infrequently, and 100% sterility cannot be guaranteed.
- Convey the fact that vasectomy is a safe intervention, which is not associated with side effects or long-term diseases, according to multiple studies that support it.
Vasectomy in Men vs. Tubal Ligation in Women
Tubectomy (better known as uterine tubal ligation) is the female equivalent of vasectomy. In it, the ducts responsible for carrying the ovum released by the ovaries to the area where fertilization and implantation take place are cut and tied, thus seeking to prevent pregnancy.
Traditionally, ligation has been more practiced in the world than vasectomy and it is likely that this is due to cultural reasons such as the old paradigm that “women are in charge of planning reproduction and ensuring their sterility.”
However, and despite the fact that it is less performed, vasectomy is simpler and cheaper than uterine tubal ligation (or tubectomy) and presents a failure rate 30 times lower and 20 times fewer complications than female surgical contraception.
Vasectomy was born as an even better alternative to tubectomy for several reasons:
- One of them is the effectiveness and simplicity of the intervention (vasectomy can be performed in less than an hour, with local anesthesia and with a very high level of safety). Tubectomy requires hospital admission, deeper anesthesia, and longer recovery
- Another reason is more functional, for example, reversing a vasectomy is much simpler and cheaper than doing it with a tubectomy
- The last one is economic. Tubectomy costs more than twice as much as vasectomy.
- Tubectomies also have a series of risks and complications. Not all women are candidates for tubal ligation surgery
Techniques and treatments
Indications
The main indication is to provide man with permanent contraception, it is usually performed in healthy patients who only seek to have control of their fertility, however, on some occasions it is performed due to the existence in the patient of transmissible genetic alterations, mental disability or other types of communicable diseases. Another of the medical indications that exists occurs when the patient’s partner has a contraindicated pregnancy, either due to high-risk obstetric delivery or other maternal-fetal alterations.
A vasectomized man is not a sick individual. On the contrary, he is a healthy person who voluntarily decides not to have more children after a simple surgical treatment and for this, this intervention should not cause any problem for the patient or his partner.
Contraindications to vasectomy
There are no absolute contraindications to the performance of this procedure, however, there are some conditions that deserve to be evaluated and corrected by the medical team in order to carry out this surgery, some of these are:
- Local infections, on the scrotal skin, epididymitis, orchitis and balanitis at the time of surgery.
- Active sexually transmitted disease.
- Coagulation disorders and hemophilia
- Gastroenteritis or systemic infections
- Inguinal hernia
- Filariasis
- Varicocele or hydrocele
- Intrascrotal tumor or mass
- Allergy to local anesthetics

Other relative “social contraindications” could be: under 30 years of age, not having children or having any relationship with a partner when deciding on the procedure.
Techniques and treatments
Surgical techniques
The vasectomy seeks to achieve the discontinuity of the vas deferens, this can be done on an outpatient basis and under local anesthesia, however, general anesthesia can benecessary for specific indications.
To achieve the discontinuity and occlusion of the ducts, different techniques can be applied:
- Excision of a piece of vas deferens and ligation with sutures or clips.
- Interposition of tissue to prevent possible recanalization
- Cauterization of the canal lumen
- Ligation with absorbable or non-absorbable sutures.
- Coagulation (electrical mono, bipolar or thermal).
- Applying clips
Vasectomy is one of the most common surgical procedures in the world. It usually lasts less than half an hour and the complication rate is very low.
Different techniques to carry out vasectomy
There are a couple of techniques that allow access to the vas deferens, which will later be occluded and sealed. This is a vasectomy. The techniques are as follows:
1. Conventional (Schmidt) technique, lateral, middle, longitudinal or transverse incisions:
In this technique, two incisions are made, one on each side of the middle scrotal raphe or through a single incision that allows access to both vas deferens, the objective is to reach and visualize the vas deferens, open the sheath that covers them and then section them. It is not determined whether the vas deferens should be ligated or if the lumen should be cauterized.
It is the most conventional of all and consists of making a longitudinal cut (between 1 and 2 centimeters) on each side of the midline of the scrotum to access the vas deferens on each side, previously separating it from the deferential artery that accompanies it in its path to the testicles.
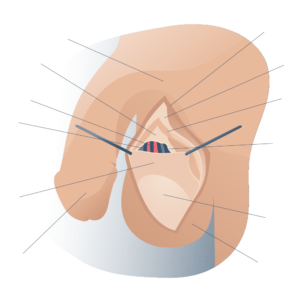
General anatomy of the testicles
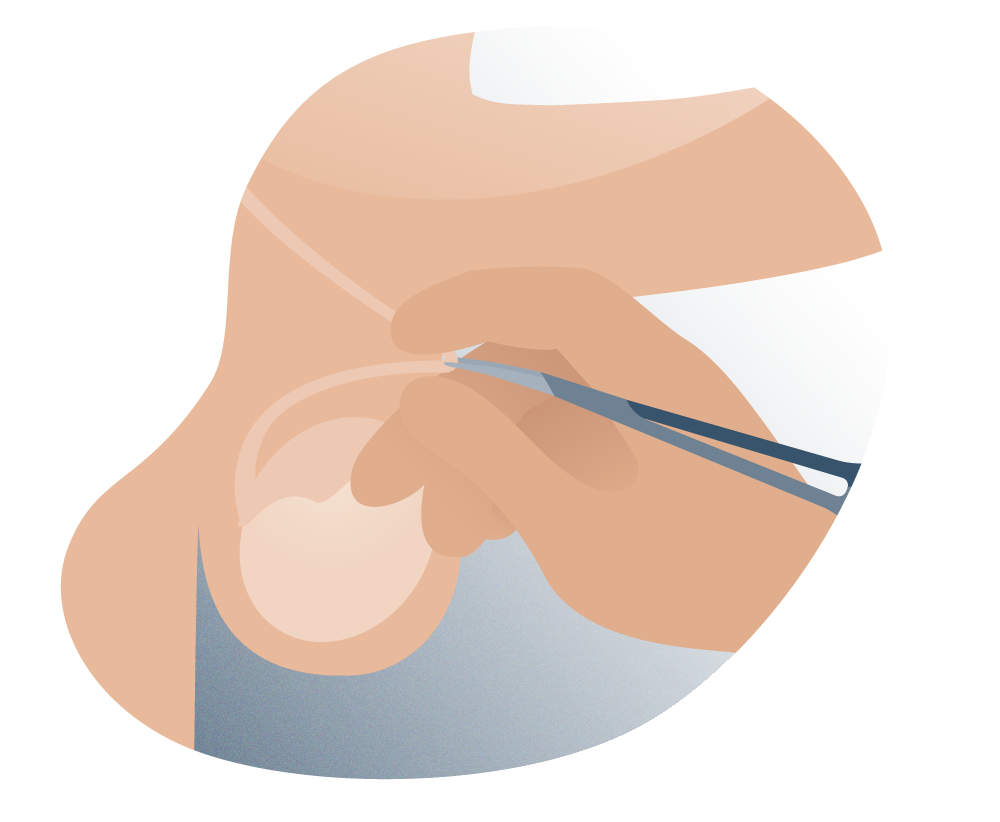
Vasectomy surgical intervention
The techniques for occlusion of the vas deferens, once identified and isolated, can vary from surgeon to surgeon (ligation, cautery, etc.). The ends of the vas deferens are then reintroduced into the scrotum and the incision is closed with absorbable suture.
The operative wound receives antiseptic ointment and is covered with gauze to protect it from friction and infections (which are quite rare, in fact).
Vasectomy surgical intervention
No-scalpel vasectomy technique
2. “No Scalpel” Technique, Percutaneous Vasectomy Technique (no scalpel, or Li Shunqiang or No-scalpel vasectomy)
It is the technique that we develop at Andromedi in the vast majority of cases. It was developed by Li Shunqiang and colleagues, in order to increase the acceptance of the procedure by avoiding the fear of incision. Here it is possible to penetrate the skin without the use of the scalpel, using special instruments, such as a forceps with a thin tip that will allow it to enter inside the scrotum and another to hold the vas deferens, frequently no cutaneous suture is needed since the eyelet that has been performed, it does not bleed and due to the same contraction of the skin, its correct healing occurs.
This technique is very minimally invasive and is widely accepted due to its low rate of early complications, such as infections, bruises, and less postoperative pain.
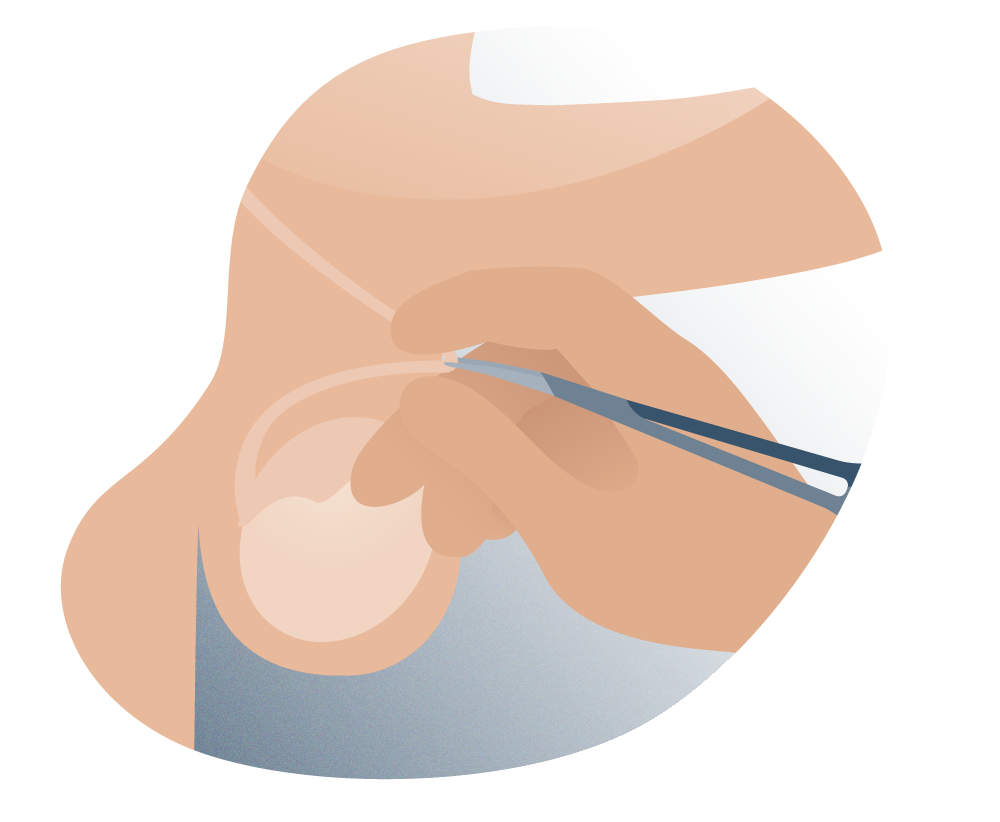
No-scalpel vasectomy technique
This technique has the particularity that it uses two surgical instruments to access each vas deferens without making any incision in the skin: a ring forceps and a mosquito forceps.
From outside the scrotum, the surgeon fixes the vas deferens with his fingers and immobilizes it with the ring clamp. There he proceeds to puncture the skin of the scrotum with the delicate sharp end of the mosquito forceps, until he reaches the vas deferens in question. After sectioning and occluding it, the surgeon returns it to the interior of the scrotum.
Because this technique does not require large incisions but instead takes advantage of a small open point in the skin, the closure of this is done with a single stitch, or even without suture. This minimizes the risk of infection or scarring. It is practically imperceptible to the naked eye.
What differences are there between one technique and another? Which is better?
Both techniques (Schmidt and Li) differ in the way of accessing the vas deferens (which carries sperm from the testicles to the ejaculatory ducts). The first of these techniques uses a longitudinal and open incision on each side of the scrotum, while the Li technique only requires a single opening point (less than 5 mm in diameter) in the middle raphe of the scrotum to allow the surgeon to reach the vas deferens.
The Schmidt technique is by far the most practiced technique in the world because it facilitates the surgeon’s task. However, in recent years there has been a great boom with the Li technique, better known as we have said as “no-scalpel vasectomy.”
Many men suffer from fears of being operated on with scalpels in thegenital area and prefer that the incision be the smallest and leastinvasive possible. For this, the Li technique is especially recommended.
No-scalpel vasectomy is less invasive, and usually has a postoperative period with fewer complications and more bearable, with less discomfort and a faster return to work.
We could summarize by saying that the no-scalpel approach technique is more modern and better, but only when the surgeon controls it and has experience. If you don’t have it, better opt for the traditional one.
Where exactly is cut in vasectomy? Where is the incision?
With the traditional technique (the Schmidt technique), two small cuts are made on each side of the scrotum, a few centimeters below the base of the penis. The stitches are made with some absorbable material, so it is not necessary to go to the doctor to remove stitches or scars remain.
The Li technique (or vasectomy without a scalpel), unlike the first, only requires a single opening point to access the vas deferens. It is usually in the middle scrotal raphe. There is no incision in the skin but a point, so the scar it leaves is minimal.
Where exactly are vasectomy scars located? Are they very visible?
Depending on the technique, the marks left may vary in location. For example, with the Schmidt technique the incision marks will be on each side of the midline of the scrotum and with the Li technique, the tiny opening will be near or above the midline.
In any case, the external appearance of the scrotum tends to make these imperfections on the skin little visible and possible scars are not very visible.
What are the most widely practiced occlusive methods of the vas?
These methods are numerous and can vary depending on the surgeon who practices them and the needs of each patient. Here we will address the most employed.
The simplest and most practiced method in developed countries. It consists of removing a small segment of the vas deferens (less than one centimeter) and tying both ends with some non-degradable material such as synthetic silk or a paper clip.
Once the vas deferens is occluded, each end can be closed individually, interposing a little of the spermatic fascia (one of the layers of tissue that makes up the scrotum and that covers the spermatic cord, through which the vas deferens, the deferential artery, runs and the venous plexus).
This maneuver tends to decrease vasectomy failure (which is already extremely low) but adds a bit of technical difficulty to the procedure.
This method has increased its use by 50 percent in the last 10 years because it has a very high success rate, compared to traditional methods.
This occlusive method consists of administering external energy (thermal or electrical) through two needle-tipped electrodes directly into the vas deferens to coagulate the deferential mucosa.
It is a technique that was also developed by Dr. Li Shunqiang, it has the same principle of the technique without a scalpel, but this uses the injection into the lumen of the vas deferens of a compound of phenol and cyanoacrylate, this product coagulates and forms a plug in the lumen blocking the passage of sperm.
The disadvantage is that it has a higher failure rate than vasectomy, and the toxicity or carcinogenicity of the product in the body has not been ruled out.
The wound should be kept clean and dry, and cold may be applied to the scrotum to help reduce pain and swelling. The patient is also advised to wear tight-fitting underwear after the procedure to reduce possible pain and swelling in the area.
Techniques and treatments
What possible complications could happen?
Vasectomy is classified as one of the safest surgeries that can be, taking into account the risks that are run with conventional surgeries (such as hemorrhage). agias, infections or possible damage to other structures) where they are somewhat greater.
Among the complications of vasectomies are some bleeding in the wound area, bruises, itching in the scrotum and testicular pain.
The latter is one of the most statistically reported and is about certain discomfort in the testicles caused by increased pressure within them. It generally has a good prognosis and heals on its own within a few weeks.

Vasectomies and Penis Size: Myths and Truths
Vasectomy as a surgical procedure for the spermatic tracts does not affect the size of the penis (in terms of thickness and length) because the latter depends on the patient and is part of their anatomy. It is practically impossible to distinguish any difference between the external appearance of the genitals of a vasectomized man and one who has not undergone this procedure.
What about ejaculation?
Premature ejaculation is a problem that affects the sexual life of many men, causing the moment of ejaculation to occur in less than a minute and the sexual intercourse ends before the female orgasm. It causes discomfort in the sufferer but also in the sexual partner.
Vasectomy does not directly influence the phenomenon of ejaculation either positively or negatively. Therefore, it does not affect or condition the existence of a premature ejaculation problem. Faced with a case of this sexual pathology, it is advisable to turn to a specialist to find a solution.
Does it cause any effect on the prostate?
Inflammatory processes of the urinary and seminal tracts (such as prostatitis) or infections are usually the product of some invasion of pathogenic bacteria in these tissues, but not as a result of the patient being a vasectomized. Studies carried out in these groups of patients, taken at random, indicate that there is no direct relationship between suffering from prostatitis (inflammation of the prosthetic gland) or STIs (urinary tract infections) and having undergone a vasectomy.
Vasectomy and Hair Loss?
Alopecia (or hair loss) in men is considered one of the most frequent diseases associated with age. After the age of 35, many men begin to experience progressive but persistent hair loss and general weakening of the scalp, giving rise to so-called “recesses” and a circular area above and behind the head (alopecia areata).
Being vasectomized is not a risk factor for developing alopecia, because it does not interfere with the production of male hormones, a key element for hair to weaken and fall out (hormonal factors associated with age).
In fact, in patients who are suffering from chronic prostatitis and germs colonize the testes through the vas causing epididymitis or recurrent orchitis, a vasectomy is recommended.
Preparations for the vasectomy procedure: What should I do?
The preparations for the vasectomy go through a good previous hygiene, such as keeping the genital area clean and shaved. This is key to attending the surgical intervention.
Similarly, there may be other prior care of the patient that is usually taken into account by the treating physician in the consultations for examinations and preoperative reviews.
For the itervention to be successful, it is important that the patient who is going to undergo it notifies the surgeon of any drug allergies, infectious disease they suffer or any health problem that they may be suffering or medication that they consume on a regular basis.
Among these drugs, anticoagulant drugs (such as warfarin or aspirin), which could condition excessive bleeding, and any antibiotic (which would indicate an infectious process prior to surgery) are especially delicate.
If applicable, these prior consultations will also include specific tests for hypersensitivity to anesthesia in order to prevent an allergic reaction in the event that there is a previous history.
The day of the intervention, although it is not essential, it is recommended to attend accompanied by a family member or acquaintance.
• Post-operative care
The patient is recommended to rest completely the day after the operation, with subsequent return to their daily activities, however, it is indicated not to have sexual intercourse for at least 3 days after the intervention, in addition to abstaining from sports or physical exercises for a period approximately 4 to 6 weeks.
It is indicated to keep the wound clean and dry, being able to apply cold on the scrotum to help reduce pain and inflammation. The patient is also instructed to wear tight underwear after the intervention to reduce discuss possible pain and swelling in the area.
How did the vasectomy come about? A little of you history.
Since ancient times, the Greeks already knew that the testicles were the organs of virility and fertility of male mammals, including humans, and that their extraction decreased male sexual characteristics and lowered levels of irritability.
However, castration was never a contraceptive method for men due to its great hormonal implications (this is where testosterone is produced) and it was only limited for therapeutic purposes, as in tumors, several centuries later.
At the beginning of the last century, many doctors began to seek male contraception by different methods, some more uncomfortable and useless than others, until the idea arose that if the tubes through which the testicle carried sperm to the urethra were divided or ligated, it was possible to ejaculate non-fertile semen with the total preservation of the endocrine function of the gonads.
However, no specific surgical technique was found and with the emergence of female contraceptives, the idea of male contraception moved to a second or third level of importance in medical research.
The Schmidt technique was devised by the surgeon who bears his name in the early 1970s in the United States. It is still the most widely used surgical technique in the world as it offers a greater range of action to occlude the vas deferens.
On the other hand, the Li technique (or no-scalpel vasectomy, VSB) was created and developed by Dr. Shunquiang Li in China in 1974, but it was not until the early 1990s that Dr. Marc Goldstein introduced in the West and promoted it, thus revolutionizing the way in which vasectomies were performed.
The Li technique is so widely accepted within the medical community that it is considered the gold standard or procedure of choice according to the American Urogical Association of the USA. This is because it is faster, with less pain and less incision, bleeding and complications (10 times less than the conventional one). At Andromedi, it is currently the one that patients demand the most from us.
Questions and Answers
Frequently asked questions at the Andromedi centres in Madrid, Seville and Tenerife
Vasectomy is by far the most effective permanent contraceptive method available to men. It could be compared in effectiveness with uterine tubal ligation, but with less surgical aggression and with an even more positive outlook.
Rates of early failure (pregnancy within a few months after surgery) are very low and result from unprotected sex that is too early.
When the vas deferens is sectioned and closed, the passage from the lower to the upper end is interrupted, but sperm remains may remain in the upper part that come out in successive ejaculations. Some traces of sperm can remain inside the upper end of the vas deferens and be ejaculated together with the rest of the seminal secretions, giving rise to an unplanned fertilization.
These vasectomy failure rates can vary from study to study but generally do not exceed 1 pregnancy for every 1,400 vasectomized men.
It is important that for at least two three months after the vasectomy (depending on the frequency of ejaculations), the couple continues to use contraceptive methods (such as latex condoms or pills) to avoid unwanted pregnancies due to seminal emissions with sperm.
The reality is that vasectomy is the safest method of contraception. The vasectomy failure rate is only 2 for every 1,000 operated. This is in contrast to the uterine tubal ligation failure rate (in women), which is 8 per 1,000 female patients.
This type of surgical intervention is covered by Social Security but not in all cases. It must be indicated and justified by a urologist from the Public Health System.
Fortunately, vasectomy is a painless surgery that causes little or no discomfort. These discomfort yield to paracetamol-type analgesics.
Very rarely, a specific pain could appear, the so-called post-vasectomy pain syndrome, which is a pathology that occurs in few cases of vasectomized men as a consequence of the increase in intratesticular pressure due to the blockage of the exit of sperm.
Post-vasectomy pain syndrome is a rare complication in vasectomy men. It is characterized by discomfort in the testicle area (usually a single testicle), with persistent pain. This is produced by increased pressure within the testicle. Often the pain goes away on its own within a few weeks.
In more extreme cases, it can be solved by releasing the end proximal to the testis from the vas deferens.
The sexual life of the post-vasectomy patient is completely normal and will not be affected at all. Your erections, orgasms, and ejaculations will continue as usual. Like his sexual desire, they will continue to be the same as before the operation.
In fact, a decrease in sexual desire has not been observed in men undergoing vasectomy, quite the opposite. On the contrary, if anything, the couple can feel more freedom and confidence when it comes to enjoying sex because there is no persistent concern to prevent pregnancy.
Often times these cases of decreased libido are caused by parallel but not associated emotional disturbances, such as anxiety and chronic stress these problems have treatment.
However, the amount of semen after the operation will only be reduced a little: about 5% but keeping the usual characteristics. Only with the use of a microscope is it possible to visualize the absence of sperm in the seminal fluid.
It is recommended not to have sex for at least two to three days after the vasectomy. However, as soon as the discomfort disappears, the patient can resume his sexual life.
Although ejaculation is a natural response of men to sexual arousal and closely related to the reproductive function of the testicles, it is not seen in the least as affected after a vasectomy. Ejaculations are still normal in terms of intensity and seminal volume.
Three days is the recommended minimum time to abstain from post-vasectomy sex.
Also, it is recommended to use a jockstrap for the genitals for five days (even at night) and the placement of cold in the scrotal area to reduce edema or swelling in the first 8 or 12 hours in the case of produce. Usually not necessary.
Although vasectomy is considered an irreversible technique, at present there is the possibility of reversing it, through the vasovasostomy technique, recanalization of the vas deferens is achieved.
The success of this procedure will depend fundamentally on the quality and quantity of the sperm (with regard to conception by natural means) and the technique used in the initial operation, the greater the amount of vas deferens that was resected, the less be the success of rechanneling.
It is often said that the elapsed time of the vasectomy also contributes, a time greater than 10 years is also associated with a lower probability of success, something that in our long experience in the operating room has not happened.
Vasectomy does not offer any protection against sexually transmitted diseases, so it is recommended to take other measures such as the use of condoms, reducing or avoiding multiple sexual partners and in more extreme cases sexual abstinence.
The price varies depending on the hospital where the procedure is performed and the medical fees, however, the cost (all inclusive) in our Seville office is approximately 1000 euros
Vasectomy does not affect any male sexual character, since the release of male hormones that are produced in the testicles, continues to occur normally and in the usual amount. These hormones are released directly into the bloodstream and are not seen n interrupted by the cutting of the vas deferens.
Therefore, the belief that vasectomy produces erection problems, feminine traits in men, and that it sharpens the tone of voice is a myth.
After vasectomy, Leydig cells within the testes continue to secrete testosterone in normal amounts into the bloodstream, without any problems.
Vasectomy interrupts the normal path of sperm (produced in the testicles) towards the ejaculation pathways, but it does not inhibit the production of male hormones (the most important of which is testosterone) that go directly into the systemic blood. This means that this contraceptive procedure has no effect on the endocrine balance of the patient.
In general terms, vasectomy does not affect the probability of developing cancer (in any modality) because the latter depends on a large number of factors, including genetic predisposition and lifestyles.
Fortunately, no scientific studies have proven the hypothesis that vasectomy increases the risk of cancer, making it a safe and harmless procedure.
Nor is it associated with heart disease or atherosclerosis with this procedure, which is why the World Health Organization considers vasectomy very safe and without long-term complications.
After a vasectomy, the sperm produced by the testicles remain within the seminiferous tubules until they mature and are reabsorbed by the body itself. These sperm are usually immobile for a long time before being eliminated.
The seminiferous tubules are thin hollow tubes in which sperm develop and mature, within the testes. This occurs from when a man enters puberty until he dies. The production of the clogged tubule slows to a near stop. After vaso-vasostomy, production is reactivated.
Because the seminiferous tubules are a sterile environment, the sperm (which are male sex cells) stay longer than usual inside the testicles until they are reabsorbed by the walls of the seminiferous tubules without the development of any infection or without origin. an inflammatory process.
Depression is a complex emotional alteration in which the sufferer has serious problems being focused on the present, making decisions or feeling enthusiasm for the experiences that he lives.
Vasectomy by itself does not cause depression because the levels of male hormones in the body are not imbalanced. However, it is probable that some patients in the history of medicine have been able to affirm that they have developed certain depressive disorders on understanding that they have lost voluntarily and later regretfully the ability to be fertile.
It is important that each man who decides to be vasectomized knows all the implications of the intervention itself and that he expresses his decision through an informed agreement of confidentiality, information and consent
Vasectomy is a surgical technique that seeks to help men to have no offspring by changing the internal morphology of the tubes responsible for carrying sperm to the penis, in a permanent and non-reversible way (not by itself).
If a vasectomized man voluntarily decides to regain his ability to fertilize a woman again, he must undergo another surgery: a vasovasostomy. An estimated 2 percent of vasectomized individuals (within a 10-year period) regret having had a vasectomy. And this figure is currently increasing due to partner changes, reaching 10% of vasectomized men who regret throughout their lives and wish to reverse the situation and have children again.
With vasovasostomy (or vasectomy reversal surgery) the ends of the vas deferens are re-permeabilized so that sperm can be found again in the ejaculation.
There are reported cases, especially in past decades. However, they should be considered as very very rare eventualities. They are completely anecdotal statistics, something like one in tens of millions, and always as a consequence of choosing a surgeon without much experience.
Vasectomy reversal can only be done with surgical procedures (vasovasostomy). No medicine or natural remedy can reconnect the extremities of the vas and restore fertile capacity to a vasectomized.
At Andromedi we receive patients from all over Spain and European countries such as Portugal, the United Kingdom or Germany, with an average of more than 100 cases per year.
At Andromedi we receive patients from all over Spain and European countries such as Portugal, the United Kingdom and Germany, with an average of more than 100 cases per year.
How much does a vasectomy cost?
Prices and financing
How much does vasectomy cost? It is very expensive?
The price of the vasectomy intervention is € 1000. This figure is fixed cost, that is, it includes everything from the beginning to the end: previous consultations, hospitalization, surgical intervention, personnel expenses, expenses of materials or operating room, subsequent check-ups or cures.
Perhaps in other centers you can find a lower price for the same operation, but we advise you to be aware of the fine print or the extra expenses that you could incur. Some clinics hide behind the fact that the price they give is “solely for their emoluments”, without understanding what, in our opinion, the patient really demands: transparency at all times, through a global figure to know “how much the cost will cost me. vasovasostomy ”.
Can it be financed in installments?
In our centers in Madrid, Seville and the Canary Islands (Tenerife), the amount of the vasovasostomy can be paid in comfortable installments, up to 6 months. Through an advantageous line of own financing (with the collaboration of Your Financed Medicine) you will be able to comfortably cope with the treatment without affecting your family finances.
Travelling to Spain for surgery
Patients coming from outside
The Andromedi Clinic, a good choice for several reasons.
Doing a quick search on the Internet, it is easy to see that there are not too many centers specialized in this treatment. The no-scalpel technique is offered in few centers with the best guarantees.
Andromedi’s experience allows us to confront these interventions with safety and guarantees of success. And it has caused thousands of patients to have traveled from outside our city to put themselves in the hands of Andromedi’s expert medical team. All of them seek the same thing: maximum reliability, safety and quality at a competitive price and with the possibility of financing every month.
How is the best way to plan my trip?
Maybe you need more information? Is there something that worries you and you are still not completely convinced? Do not hesitate, write to us without obligation through our contact page. We would like to be able to help you, and more importantly, we know how to help you.

· We are used to thinking of you ·
We are used to thinking about you: your needs, your fears, your doubts and your problems. We could not prepare an intervention with patients from other places other than by putting ourselves in their place at every point of the process. And after all, leaving your city and being far from home is like traveling from further afield, there is not much difference.
The Colón Medical Center15, the space where Andromedi’s main practice currently resides, is located in Seville (Spain), one of the most beautiful and touristic cities in Europe, chosen multiple times with the award of the “best city in the world to visit”.
The San Pablo-Seville Airport maintains direct air connections with 52 different destinations, being able to make an international stopover with Madrid or Barcelona if necessary. In turn, the High Speed train is an agile way to move around the interior of the country, connecting the most important cities in a matter of hours.
It is not surprising, therefore, that many of these patients choose to take their vacations with a double purpose: that of being able to visit a unique enclave and that of undergoing surgery by one of the greatest specialists in Urology in Europe.
There are other occasions, in which if the patient requires it for work or personal reasons, we also have a special protocol of “rapid intervention” in which we minimize deadlines and procedures (both in large surgeries with admission and small ones), which includes The next points:
the weeks prior to the trip, in order to gather all available medical documentation ible and plan the intervention.
with the transfer and stay in our city, for which we have tourist partners associated with our center.
(face-to-face), more extensive and complete, which is usually done the day before the intervention, and includes the pre-anesthetic evaluation if necessary, to prepare all the details of the case.
with or without hospital admission (usually a maximum of 24 hours).
BIBLIOGRAPHIC REFERENCES
- Surgical contraception for men, Vasectomy. National Programme on Sexual Health and Responsible Procreation.
- What health workers need to know
- Ninaad S Awsare, Jai Krishnan y colbs. Complications of vasectomy. Department of Urology, Lister Hospital, Stevenage, UK. Ann R Coll Surg Engl 2005; 87: 406–410
- G.R. Dohle, T. Diemer, Z. Kopa et al. European Association of Urology Clinical Guide to Vasectomy. Actas Urol Esp. 2012;36(5):276---281
- Macarena Quesada Moreno, Silvia Inés Delgado García y Cecilia Oliver Sánchez. Male surgical contraception: Vasectomy. Spanish Society of Contraception.
- Ira D. Sharlip, Arnold M. Belker, Stanton Honig y Colbs. VASECTOMY: AUA GUIDELINE. American Urological Association (AUA) Guideline
- P. Romero Pérez, F.J. Merenciano Cortina Vasectomy: a study of 300 interventions. Review of national literature and complications Actas Urol Esp. 28 (3): 175-214, 2004
- VASECTOMY CLINICAL PRACTICE GUIDELINE EUROPEAN SOCIETY OF UROLOGY
- VASECTOMY CHILEAN SOCIETY OF UROLOGISTS
- LONG-TERM CONSEQUENCES OF VASECTOMY CF UNTINVEROS MAYORGA – 2014 Scielo
- NO-SCALPEL VASECTOMY SEPULVEDAS – 2014 Scielo
- VASOVASOSTOMÍA. Scielo ESPAÑA – 2005
- MICROSURGICAL VASOVASOSTOMY Chilean Journal of Urology
- RECANALISATION OF THE VAS DEFERENS Spanish Fertility Society.
- Author: DR. Natalio Cruz Navarro - TREATISE ON ANDROLOGY AND SEXUAL MEDICINE. Spain, 2011 - EDITORIAL MÉDICA PANAMERICANA
Author
Natalio Cruz MD, with 25 years of medical experience, has been until 2016 Head of the Andrology Unit in the Urology Service of the Virgen del Rocío Hospital in Seville, National Coordinator of Andrology in the Spanish Association of Urology (AEU) and General Secretary in the ESSM, positions that he has narrowed to focus squarely on this exciting project of offering a high-level private medical consultation in Marbella, Seville, Madrid and Tenerife.
Andromedi pertenece a las organizciones médicas más destacadas en el sector de la Uro-Andrología