FREQUENT CAUSES
What causes urine leakage?
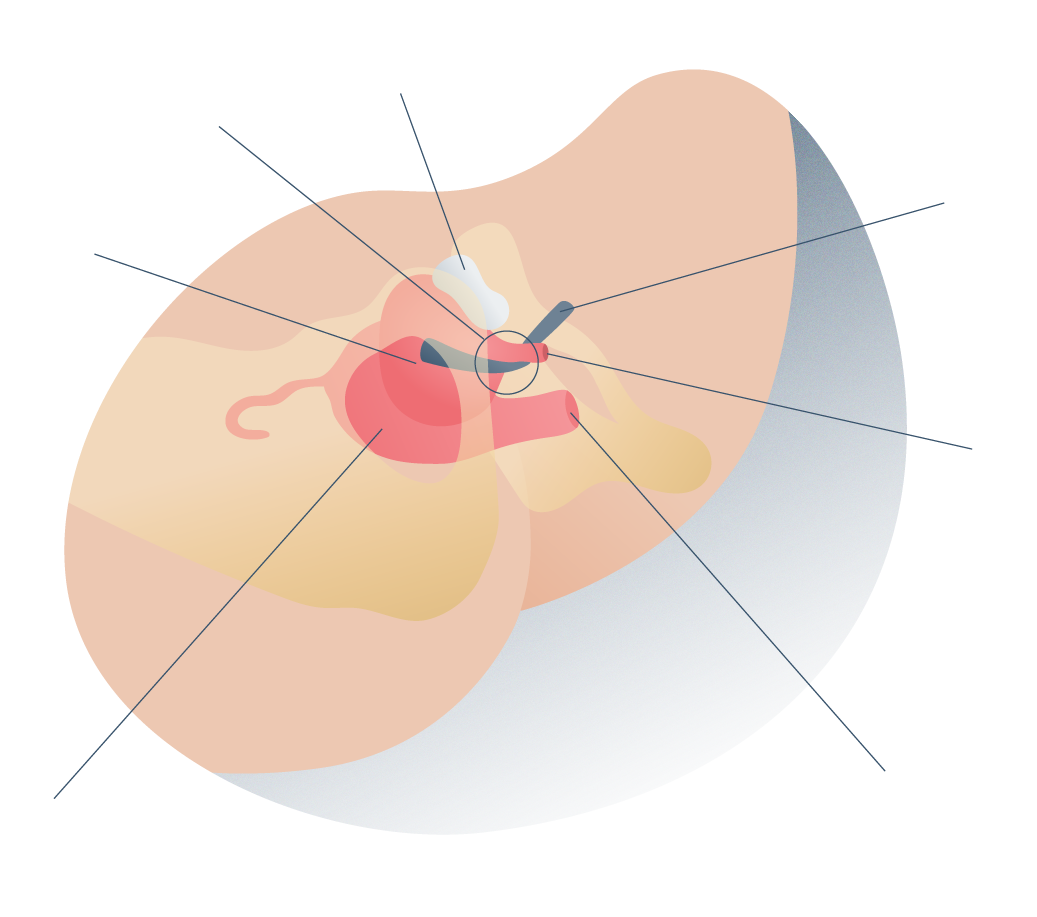
Generally, urine leakage is related to the malfunctioning of muscles and nervous tissues that enable the retention or release of urine which is produced in the kidneys and then stored in the bladder before getting to leave the body through a small tube that connects the bladder to the outside: the urethra.
The role of the muscles that make up the structure of the bladder is mainly contraction (to eject or expel the fluid). This process also involves the sphincter muscles (surrounding the urethra) which relax to allow the fluid to be expelled from the body.
The prevalence of this condition is different for both sexes as it tends to affect women more than men. Pregnancy, childbirth, and menopause are risk factors that contribute in many cases to its appearance. To a lesser extent, it can also be caused by surgical interventions, diabetes, being overweight, neurological degeneration and other injuries.
Pelvic Organ Prolapse (POP) is a pathology that is often associated with urinary incontinence in women. We have performed a few surgeries to solve complex cases that present both pathologies. Thanks to the use of polypropylene meshes in urology, patients who once did not find a definitive solution to these problems can now return to their completely normal lives.






Andromedi pertenece a las organizciones médicas más destacadas en el sector de la Uro-Andrología