Diagnosis
How do I know if my son has cryptorchidism? What are the ways to diagnose it?
The testicle considered normal is that which is visible and palpable at the base of the scrotum without any manipulation. When it is located outside the scrotum, it is referred to as a maldescended testicle.
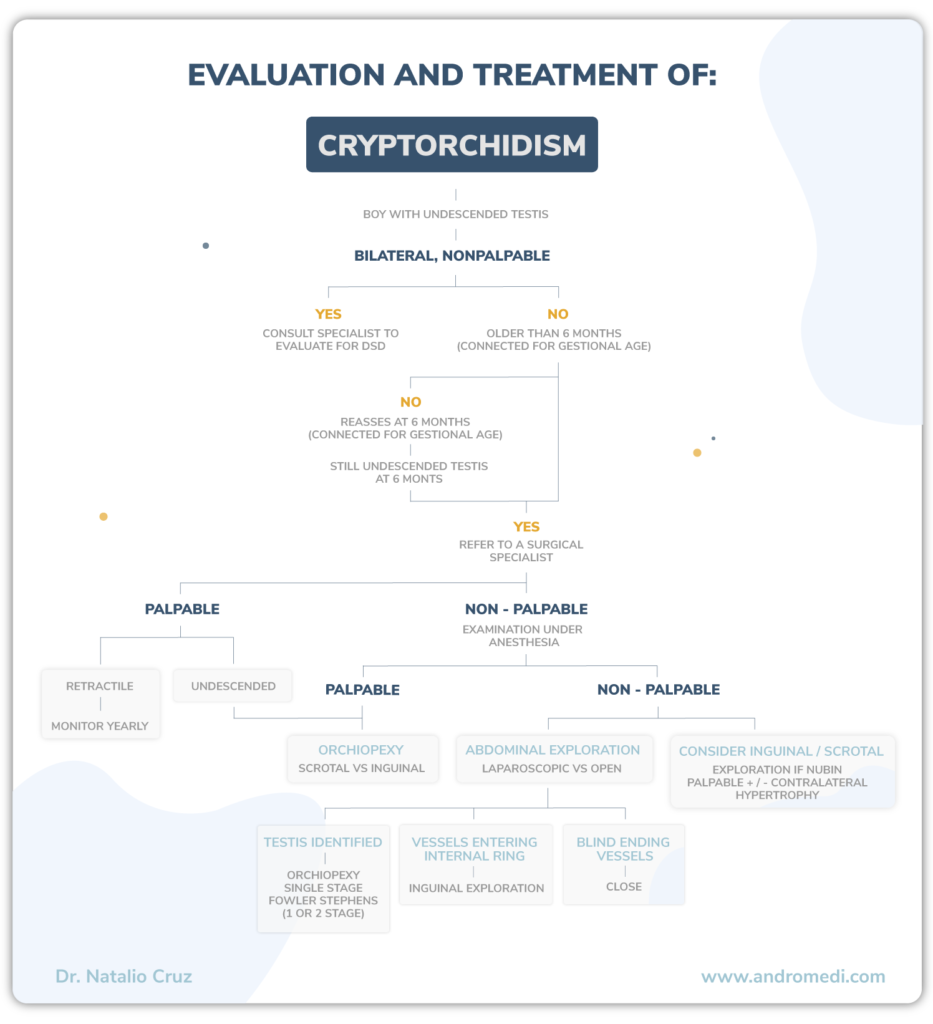
Two large groups can be distinguished according to the physical examination:
· Nonpalpable testicle ·
No testicle is found, either because it does not exist or because it is inaccessible to palpation since it would be located in the abdomen (intra-abdominal testicle).
· Palpable testicle ·
A testicle is evident outside the scrotum. It can be:
1 Palpable undescended testicle; located in the normal course of testicular descent but can not descend to the scrotum or if it does, it immediately retracts when released.
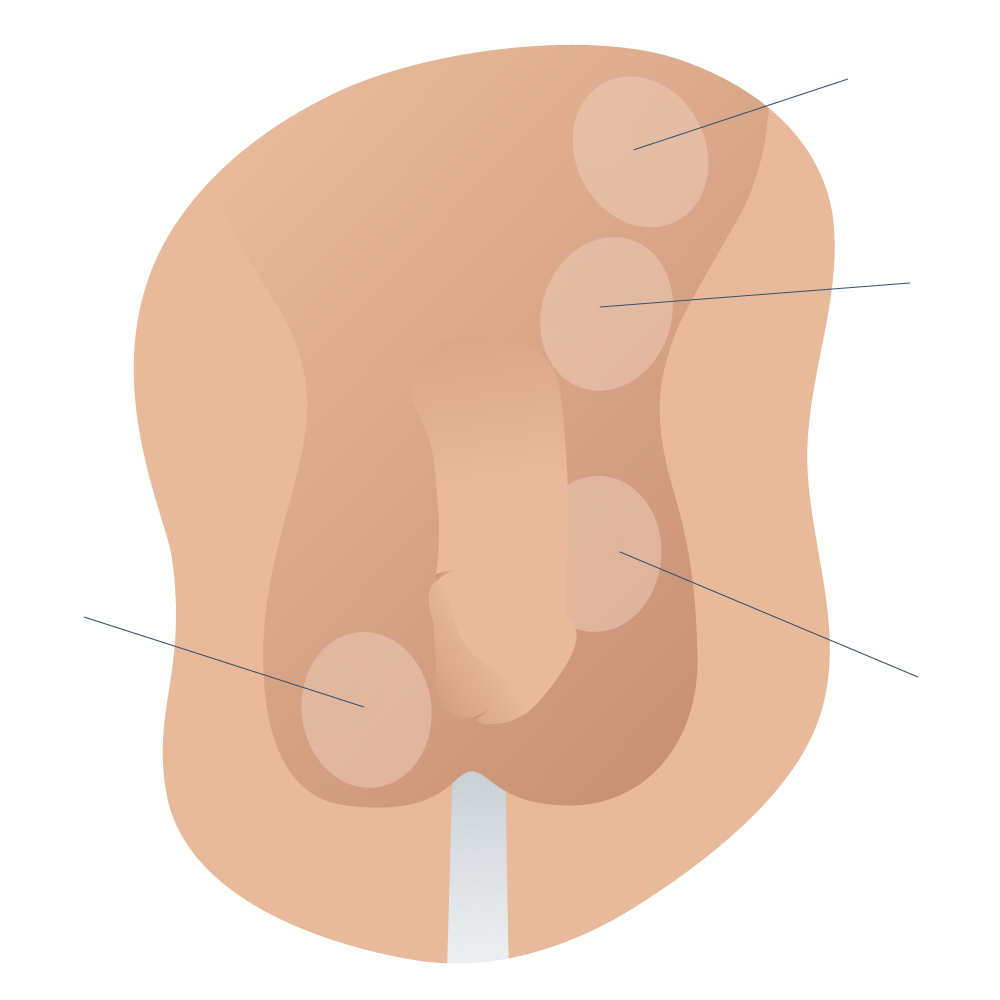
Classification of actual testicular descent in boys
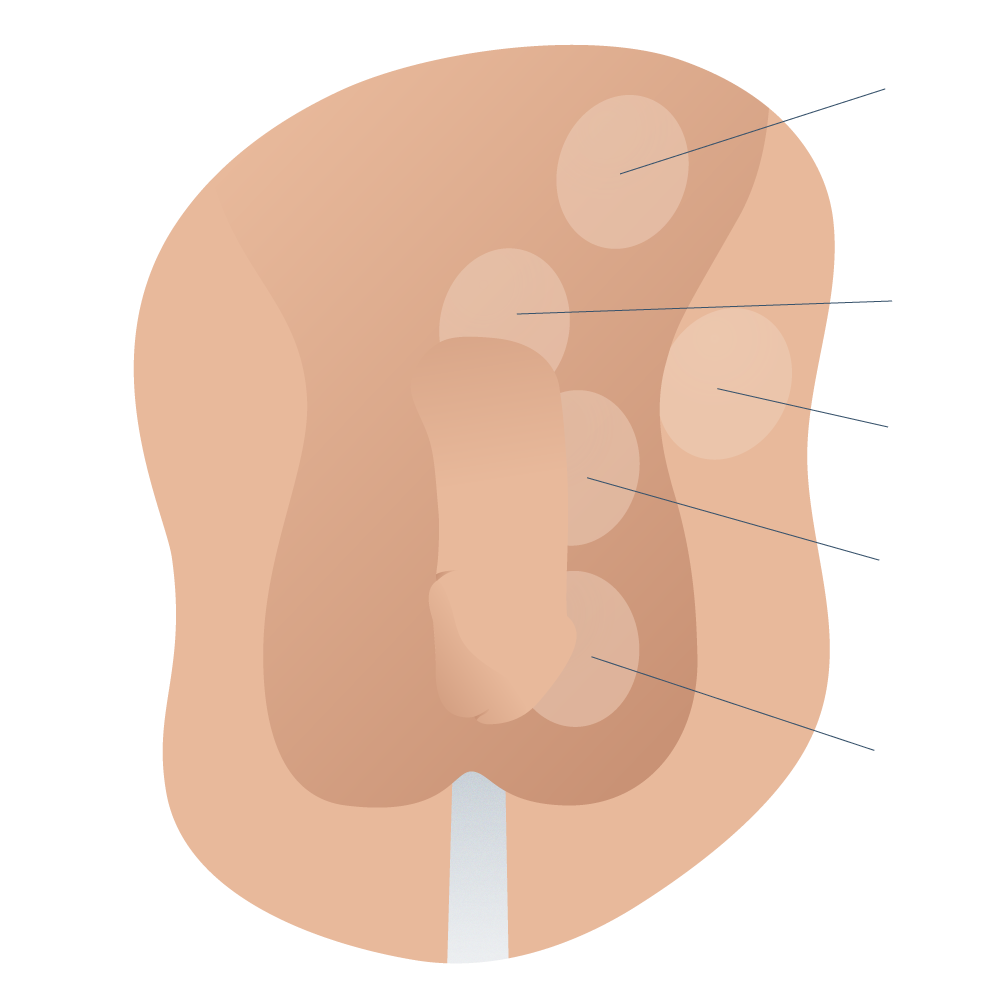
Classification of ectopic testicular maldescent in boys
2 Ectopic testicle; located out of the scrotal sac and off the path of normal testicular descent. It can be femoral, perineal, transverse, etc. The most common is the superficial inguinal i.e. a subcutaneous testicle on the fascia of the external oblique.
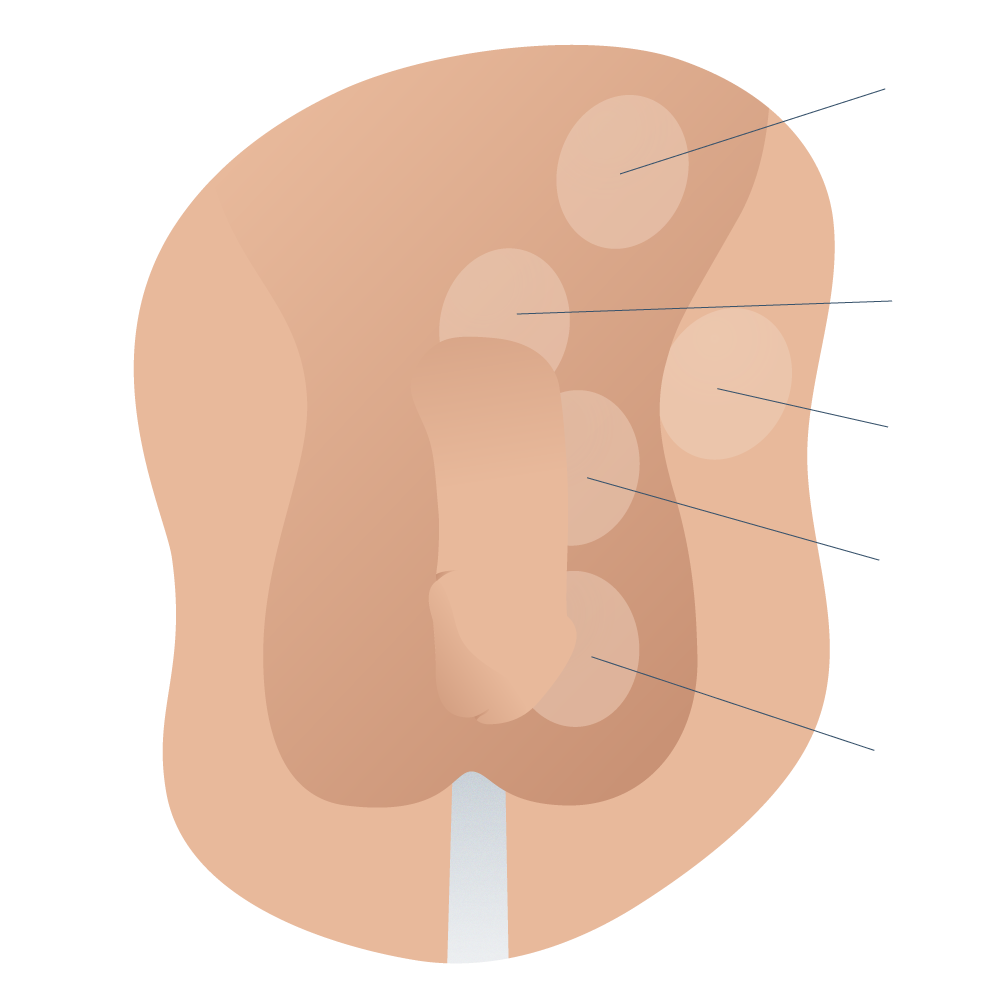
Classification of ectopic testicular maldescent in boys
3 Retractile testicle; manually manipulated to descend from its inguinal location to the scrotum. However, it ascends when triggered by the cremasteric reflex and then descends spontaneously to the scrotum when the reflex is nullified. It usually occurs between the ages of 1 – 14 years.
4 Acquired undescended testicle (acquired cryptorchidism); It is a testicle that was located in the scrotum in the first years of life and then ascended to the inguinal canal. It occurs in between 3 and 45% of cases with retractile testes.
The clinical history and physical examination constitute the fundamental pillars for the evaluation and management of children with maldescended testicles.
· Information the Doctor will ask during the first consultations ·
Background information is very important in knowing whether there are other cases of maldescended testicles in the family, in addition to details like the duration of pregnancy and birth weight. For the pediatric urology specialist, it is important to ask when the parents first noticed the empty scrotal bag, because if at birth the testes were in the scrotal sac and then later ascended outside the scrotum, the diagnosis will be retractile testicles or ascended testicles.
Physical examination
To carry out the examination correctly, care must be taken with the baby:

- Pleasant room temperature
- The child should be comfortable, calm and relaxed.
- The andrologist must have warm hands and carry out the test without haste. The best time to make the diagnosis is during the neonatal period because, at this age, the cremasteric reflex is absent or very diminished (this reflex is the one that occurs when stimulating the skin of the upper part of the thigh, causing a rise in testicle level). To locate the testicle, the most common areas of maldescent such as the inguinal, pubic/penile, femoral, or perineal region, etc. are examined.
- The initial, spontaneous situation of the test.
- Final situation to where you can manually cause the testicle to descend and whether or not it ascends again when released.
- Observe the path the testis follows in its manual descent.
- Check the size and compare with the contralateral testicle using an orchidometer.
- Development of the scrotal sac: it is often well developed in both the retractile and undescended testicles. However, some cases present with a variable degree of hypoplasia.
- Characteristics of the spermatic cord: its thickening or silkiness suggests the persistence of the peritoneal-vaginal duct or a permeable hernial sac.
- Penis: size and position of the urinary meatus.
Complementary examinations
In general, no further examination is necessary when the testes are palpable.
They are only indicated in special cases such as a “bilateral non-palpable testicle” or when a disorder of sexual differentiation is suspected (ambiguous genitalia, intersexual state, testicular hypoplasia, proximal hypospadias, a micropenis, hypospadias with cryptorchidism, etc.).
A number of indications are evaluated between two and three months of age:
Hormonal study:
- Thyroid-stimulating hormone (TSH).
- Follicle-stimulating hormone (FSH).
- Baseline luteinizing hormone (LH) (to assess the existence of Leydig cells).
- Anti-mullerian hormone (AMH) and inhibin B (to appreciate the presence of Sertoli cells).
- In children older than three months, the human chorionic gonadotropin (HCG) test will also be performed.

Other possible investigations for more complex cases include:
- Genetic study and karyotyping (chromosome analysis).
- Abdominal and pelvic ultrasound to identify the possible presence of Müllerian remnants.
- Magnetic resonance (MR) to confirm in case there is any doubt.
- Laparoscopy, which is also indicated in most of these special cases, in addition to non-palpable testing. Unilateral palpable testicle
- Ultrasound. It should not be a routine investigation because it is less reliable than a good physical examination. However, before a non-palpable test, especially in an obese patient, an ultrasound scan must be performed since it is non-invasive in addition to being highly sensitive and specific.
- Magnetic resonance angiography (MRA). The delayed phase-contrast imaging test allows us to identify the vessels of the pampiniform plexus and provides information about the anatomical situation as well as the testicular morphology.
- Laparoscopy. It is indicated if evidence of a testis is not found because it has the great advantage of being both diagnostic and therapeutic.
But, many men can suffer from some curvature of the penis without necessarily being a case of Peyronie’s disease. Because of this, there is a medical criteria to determine when a penile curvature is pathological and when it is not: the angle of the penile curve.
It is considered a pathological penile curvature when the organ has an angle of incurvation equal to or greater than 30 degrees. Less than that, it rarely causes discomfort during sex or masturbation and therefore no treatment is necessary.



 If it presents that variable behavior, it is very likely a retractile testicle, not a maldescended testicle. As we discussed earlier on this page, retractile testicles don’t require surgery, but observation and patience, because it is a condition that tends to solve by itself when the male is approaching puberty.
If it presents that variable behavior, it is very likely a retractile testicle, not a maldescended testicle. As we discussed earlier on this page, retractile testicles don’t require surgery, but observation and patience, because it is a condition that tends to solve by itself when the male is approaching puberty.
Andromedi pertenece a las organizciones médicas más destacadas en el sector de la Uro-Andrología