Pediatric urology treatments
Hypospadias
Congenital anomalies of the penis are common and can be caused by an alteration in sexual differentiation, genital differentiation or penis growth.

Hypospadias
Table of Contents

DEFINItion
What is hypospadias?
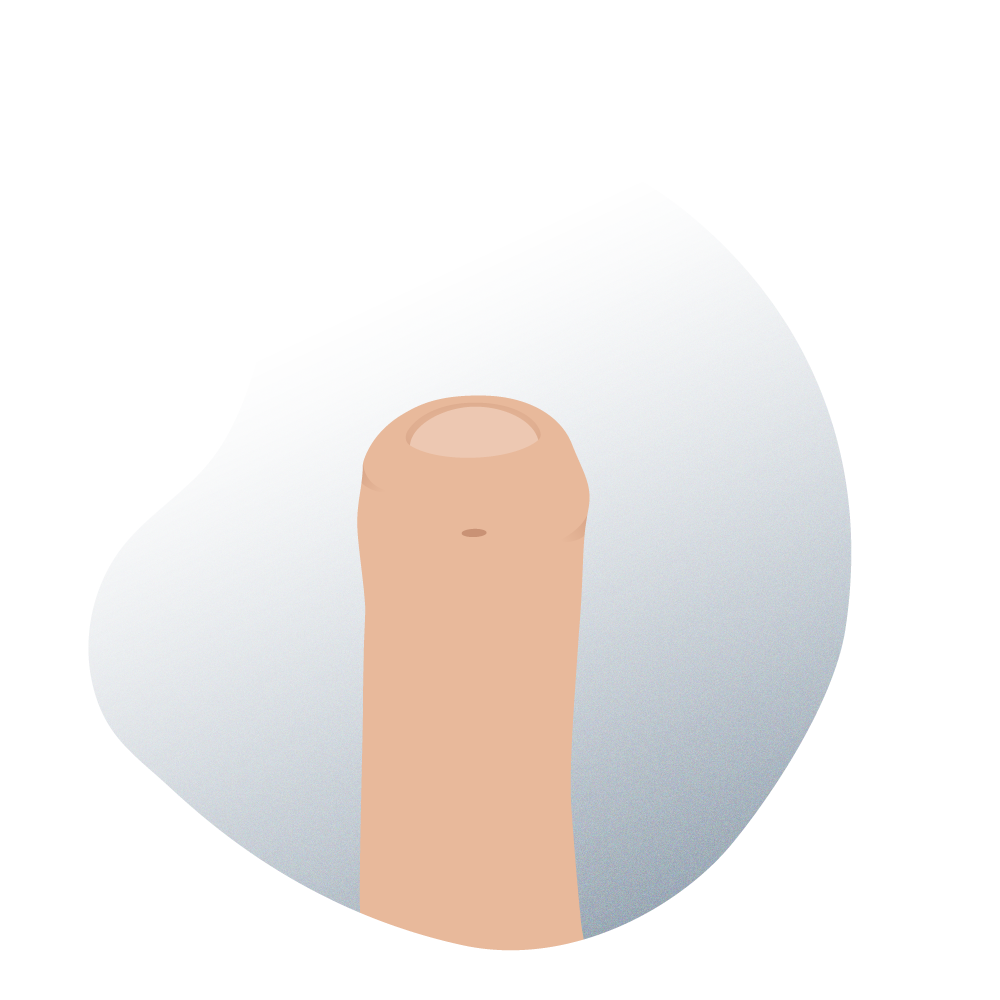
Hypospadias is the most common congenital (from birth) pathology of the penis. It can be defined as an abnormal ventral opening of the urethral meatus (in plain language, the hole through which urine is expelled) located out of place.
There are three anatomical defects associated with this pathology: In addition to the aforementioned ventral ectopic opening of the urethra (below the penis), the penis is usually curved downwards, and preputial skin absent on its ventral side. The meatus can be located at any point between the ventral side of the glans and the perineum. This is often accompanied by the ventral curvature of the penis and a deficient foreskin on its ventral side, which gives it a typical dorsal foreskin cap appearance. It must be noted that these last two characteristics may not be present in all cases.

Etymologically, the term hypospadias is derived from the Greek words ‘Hypos’ (which means ‘below’) and ‘Spadon’ (which means ‘opening’).
Congenital anomalies of the penis are common and can be caused by an alteration in sexual differentiation, genital differentiation, or in penis growth. Most cases are diagnosed at birth with a physical examination. The incidence of hypospadias varies from one country to another (between a minimum of 0.3% and 0.7% maximum). In general, it is accepted that 1 of every 300 males will present with the condition to a greater or lesser degree. The term multi-operated hypospadias refers to those patients who continue to suffer from the same medical condition despite having undergone several surgical interventions to correct it.
Although there is no scientific agreement on why it occurs, it is accepted that both genetic and environmental factors must be involved. Urethroplasty is necessary to achieve the functional and aesthetic normality of the genitals since it is of great importance because of the functional and psycho-sexual repercussions it can have on adult life even though it is a rare anomaly.
Looking for prices and information?
Use our virtual assistant and receive in your email everything related to the treatments that interest you. Budgets, recovery times, hospitalization, financing possibilities month by month, etc.
In just a few minutes and without any commitment.
En cumplimiento del Reglamento General de Protección de Datos le informamos que los datos por Vd. proporcionados serán objeto de tratamiento por parte de Andromedi con la finalidad de prestarle el servicio solicitado y/o contratado. Los datos no se cederán a terceros salvo en los casos en que exista una obligación legal. Para más información puede consultarla pinchando aquí.
Hypospadias
Treatment Summary
This is short summary of the whole process: from the appointment request, to receiving the medical discharge after the treatment in some our Andromedi centers in Madrid, Seville or Canary islands (Tenerife)
Consultations Needed
To evaluate hypospadias, at least one medical consultation is required, but for surgery additional ones are required (preoperative exams).
Hospital Stay
The child with hypospadias (the most common case) requires a hospital stay of at least three to four days after surgery.
Anesthesia Type
Local, but with sedation (induced sleep) so that the child is calm during surgery.
Operation Time
The surgery lasts between 30 minutes and one hour, depending on the degree of the anatomical malformation of the penile urethra opening.
Post-operative
The child should rest and the parents should be aware of when the child needs to go to the bathroom.
Resuming Sex Life
A boy who has had hypospadia repair surgery can do almost anything, not to mention physical rest on the initial days.
Frequent causes
Why does this urethral disease occur in babies?
This anomaly is produced by an interruption in the embryological development of the spongy tissue of the urethra, the lower face of the foreskin, the natural vertical orientation presented by the fetal penis.
Most hypospadias cases are diagnosed at birth with a physical examination and it should be noted that their most common forms are mild. The incidence of hypospadias has been increasing since the 1960s. And although this fact is partly explained because mild cases are better diagnosed, the fact is that other events such as an increase in the number of testicular cancer cases and a decrease in semen quality have also been observed in the general population, making us consider the possibility of existing environmental contaminants that influence the normal virilization of male fetuses.
The exact medical reason why this phenomenon occurs is still unknown. However, several factors are statistically related to hypospadias:
- Hormone alteration.
- Low birth weight.
- Advanced maternal age.
- Genetic predisposition by family inheritance.
There are well-founded theories that argue that the general increase in exposure to estrogen-pollutants that has been suffered by the population, as well as the increase in hypospadias in men conceived by in vitro fertilization, are probably related to the administration of progesterone. They presume the possibility of this anomaly occurring from the early stages of pregnancy due to endocrine disruption.
Between the seventh and eighth week of gestation, one of the first signs of masculinization occurs; an increase in the distance between the anus and the genital structures, followed by the elongation of the phallus, the formation of the penile urethra and the development of the foreskin. The penile urethra is formed as a result of fusion in the midline of the endodermal folds of the urethra.
The formation of the urethral plate and the modeling of male external genital tissues is a complex process in which genetics, cell differentiation, and hormonal/enzymatic activity are involved.
Types of hypostasies according to their position
Medical evaluation
Why are we talking about the different types of hypospadias?
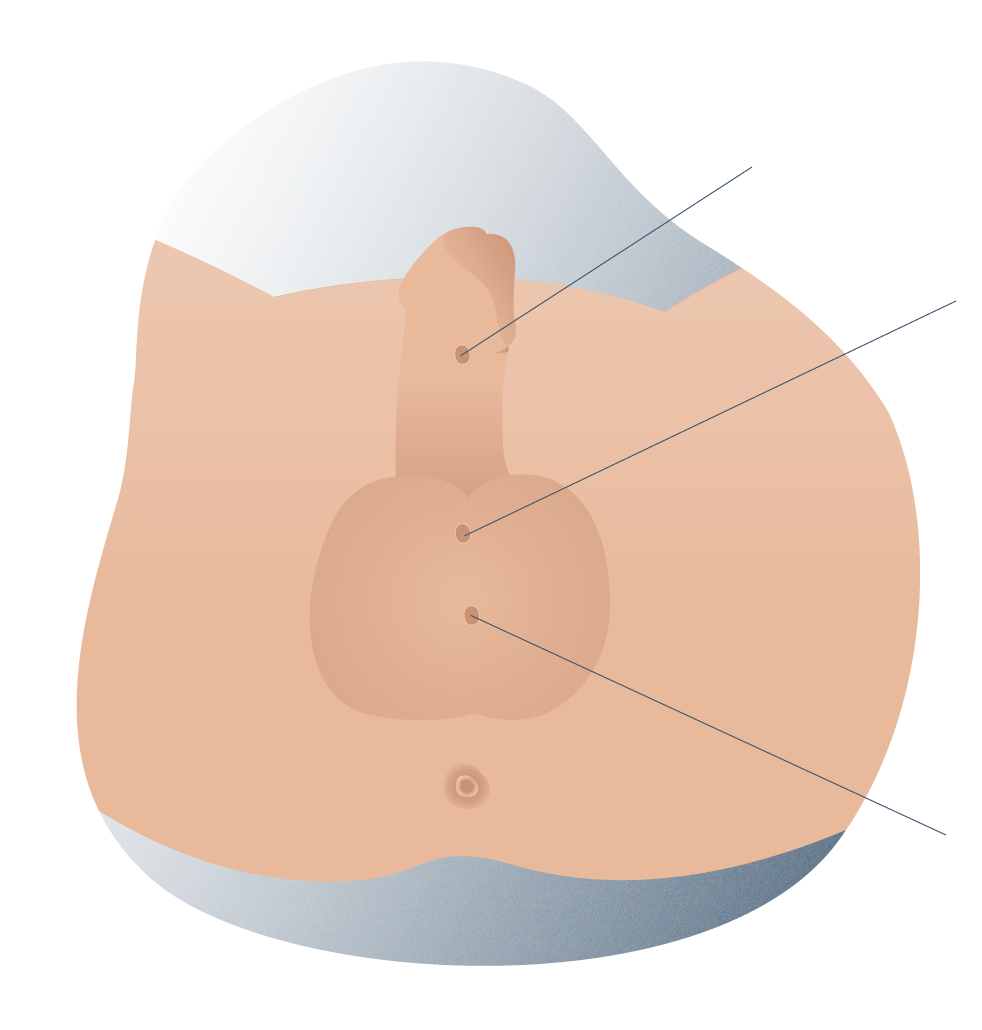
There are several types of hypospadias, which are usually described according to the position where the opening of the urinary meatus appears. However, this type of standard classification has limited value, since it can vary once the curve of the penis is corrected. Instead of using such a classification, we should describe the anatomical data covering:
- The position of the urethral meatus before and after the correction of the curvature, if present (glandular, distal or proximal).
- The characteristics of the foreskin (complete or incomplete).
- The glans (cleft, incomplete cleft, or flat glans).
- Urethral plate.
Taking into account the point where the development of the spongy tissue is interrupted, we can distinguish between the distal or anterior hypospadias (where the spongy body has been interrupted near the glans and there is a slight curvature) and the posterior hypospadias, in which the proximal interruption (near the base of the penis) of the spongy body produces a more or less severe curvature, in addition to hypoplasia of the tissues that form the ventral part of the penis.
Penile Hypospadias
Cryptorchidism and inguinal hernia are the most common associated anomalies in patients that require corrective surgery for penile hypospadias. Severe forms of hypospadias may look similar to the indications of patients with alterations in sexual differentiation.
Types of hypostasia according to their lateral position 01

Types of hypostasia according to their lateral position 02
Types of hypostasia according to their lateral position 03

Types of hypostasia according to their lateral position 04
Techniques and treatment
Surgical treatment, techniques, and results in the Pediatric Unit of the Andromedi Clinics in Madrid, Seville and the Canary Islands (Tenerife)
The only possible treatment for hypospadias is surgical correction. There are no outpatient medications or cures. The surgery must be performed by specialized surgeons who are usually dedicated to these types of anomalies. Our advice to the parents of the child is very clear; you must ensure you are advised and assisted by a specialized professional because it is a sensitive procedure which can have complications if not properly carried out.
The ideal time for the repair of hypospadias should be in the first year (12-15 months) of the baby's life. In any case, it is recommended that the surgical intervention is carried out before the child is aware of their genitals, to avoid the psychological implications that genital surgery could have on the child.
El tiempo óptimo para la reparación del hipospadias debe ser en el primer año (12-15 meses) de vida del bebé. Se recomienda que en cualquier caso se lleve a cabo antes de que el niño sea consciente de sus genitales, para evitar las implicaciones psicológicas que la cirugía genital podría tener en el niño.
Advances in the technical aspects of the surgery and the development of pediatric anesthesia make it possible for the intervention to be performed without problems at that early age. Hypospadias surgery is performed under general anesthesia and is combined with the blockade of the penile nerves or caudal block to reduce postoperative pain. It requires a pediatric anesthesiologist and a short inpatient stay in most cases.
Both gonadotropin and testosterone have historically been used in previous treatments for patients with hypospadias with the intention of increasing the size of the penis and improving the vascularization of the tissues before surgery.
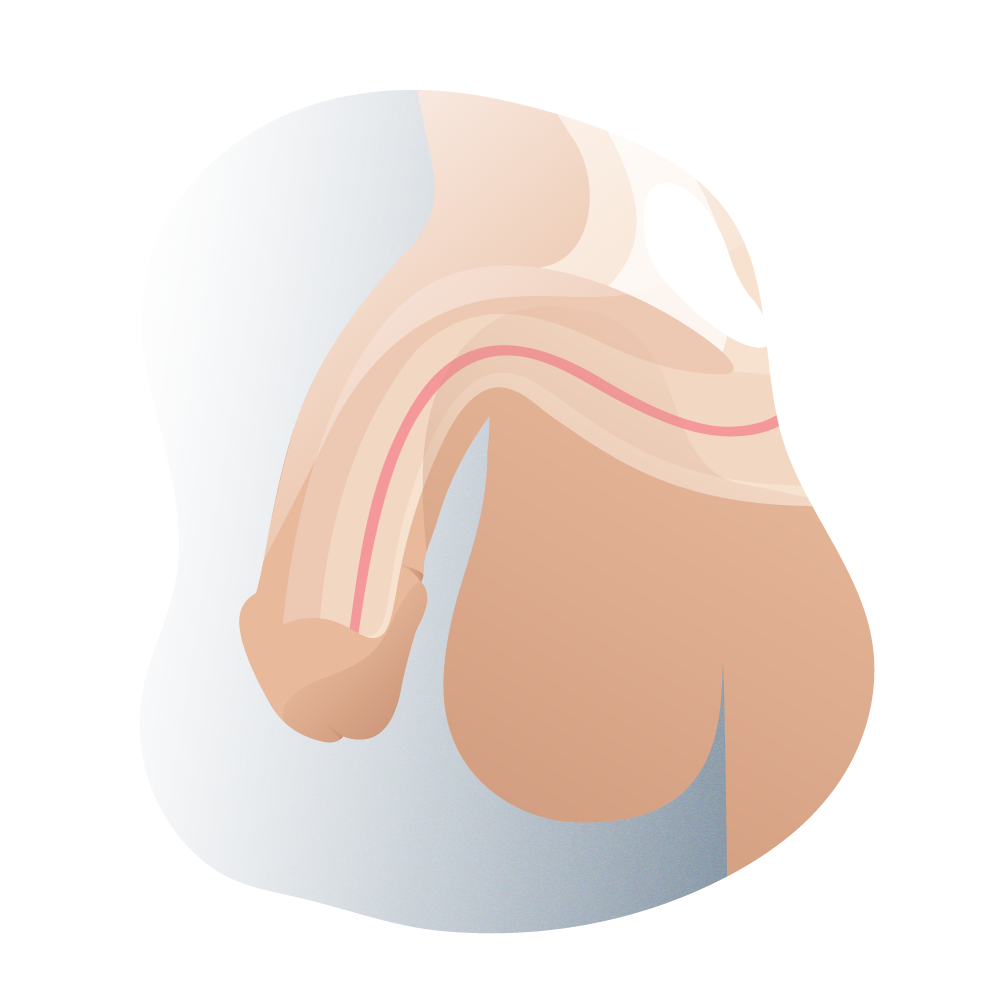
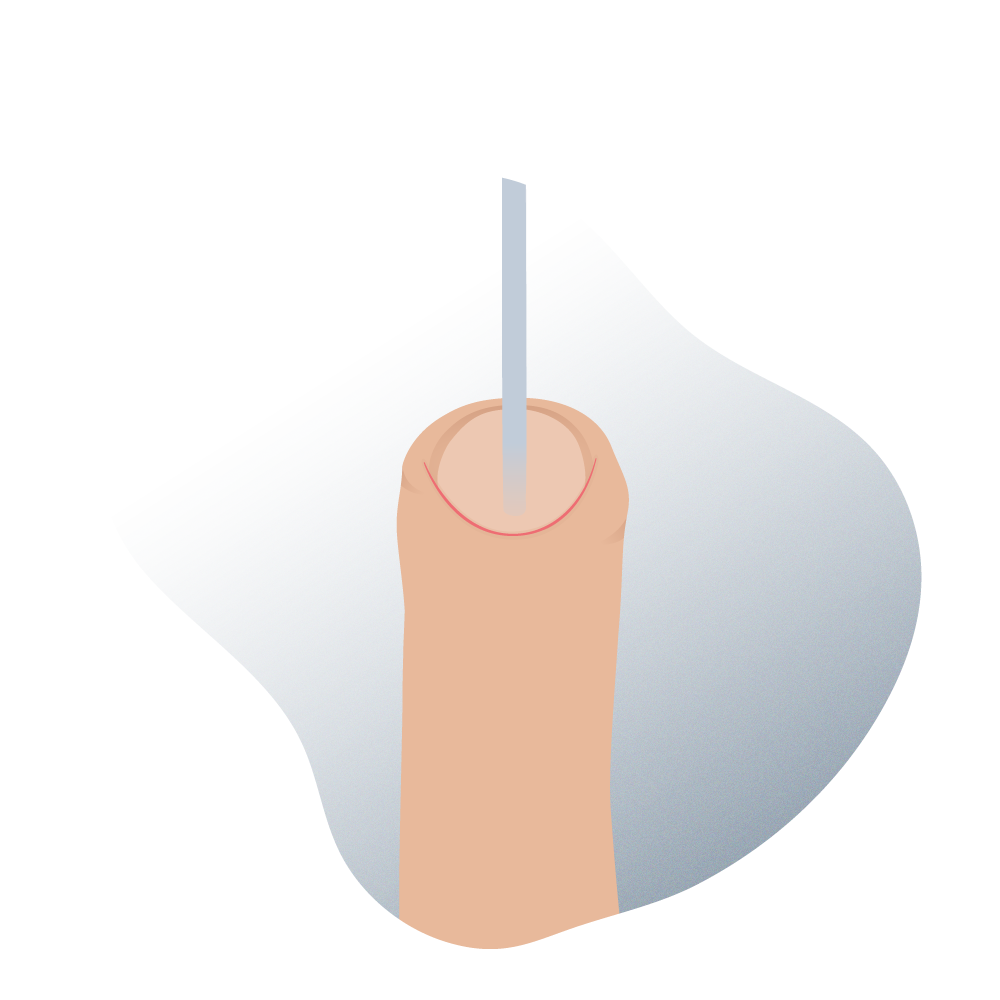
Hypostasia surgery 01
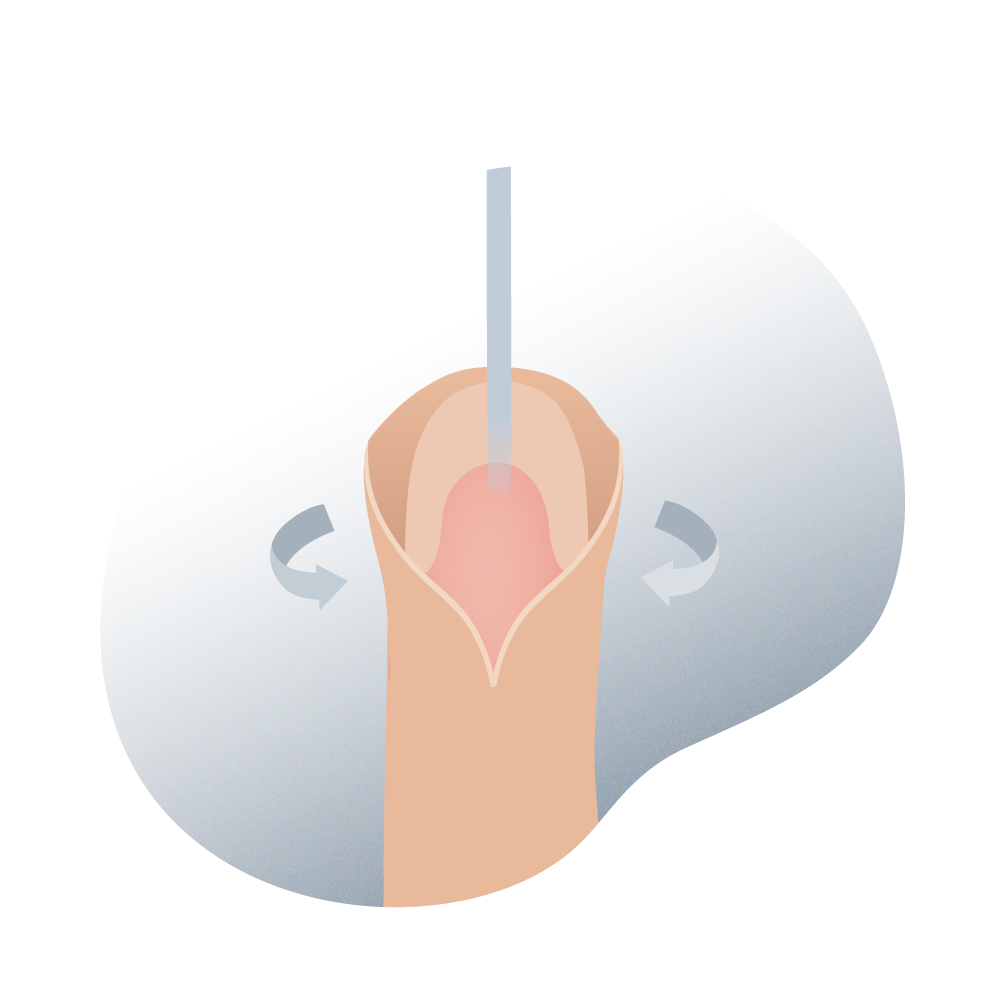
Hypostasia surgery 02
Preoperative treatment with gonadotropins is not well standardized due to the lack of consensus protocols in its administration. Moreover, it has been indicated that testosterone is more effective than human chorionic gonadotropin (HCG) in stimulating the growth of the hypospadiac penis. Testosterone cream (2% testosterone propionate) or its intramuscular administration (testosterone enanthate, 25 mg in a monthly dose, for 3 months) are possibilities to be assessed by the urologist, according to each particular case.
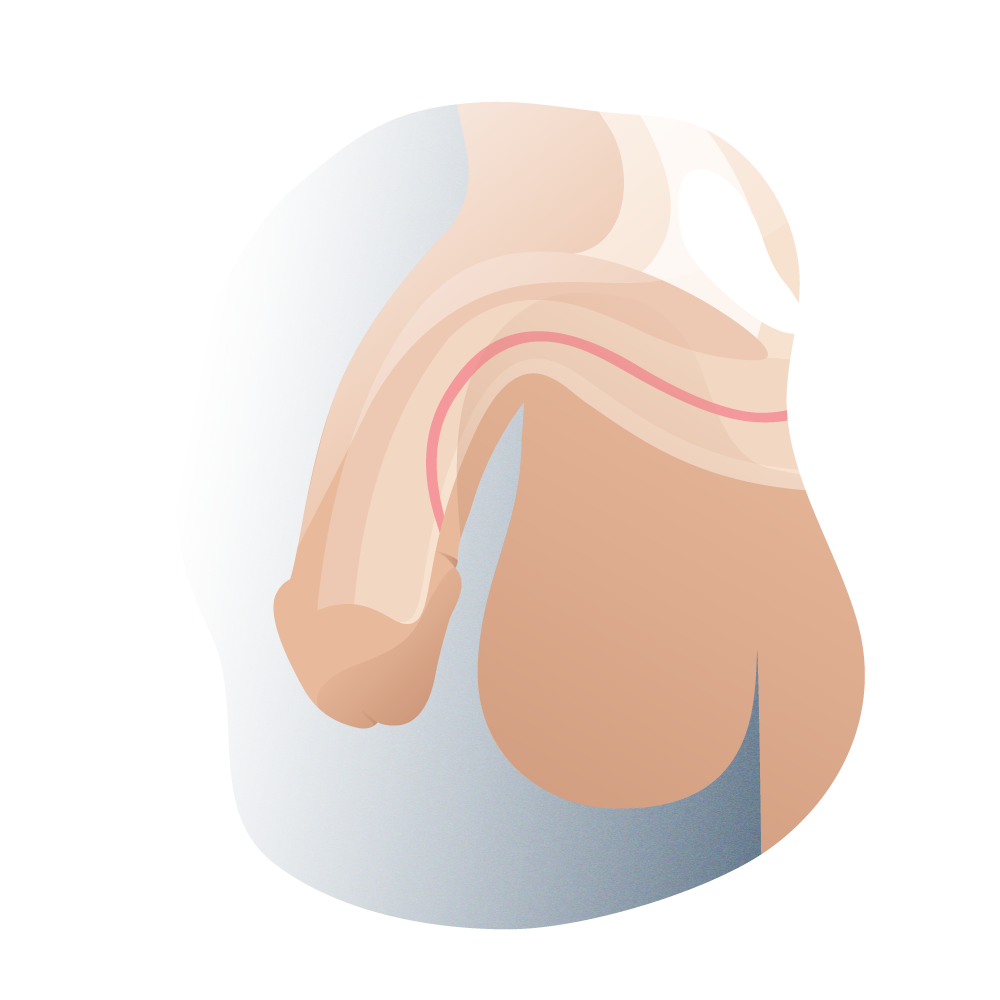
From a surgical standpoint, the fact that there are numerous techniques described for the repair of hypospadias (it is not a defined international standard) requires that each medical center and surgeon have their own experience and preferred procedure. In recent decades, specialists have come to a consensus on the objectives to be achieved in the correction of hypospadias. You must get the penis straight in erection and the urethral meatus in the terminal part of the glans, to enable the urine stream to be well directed forward while making it possible for a future of normal sexual intercourse.
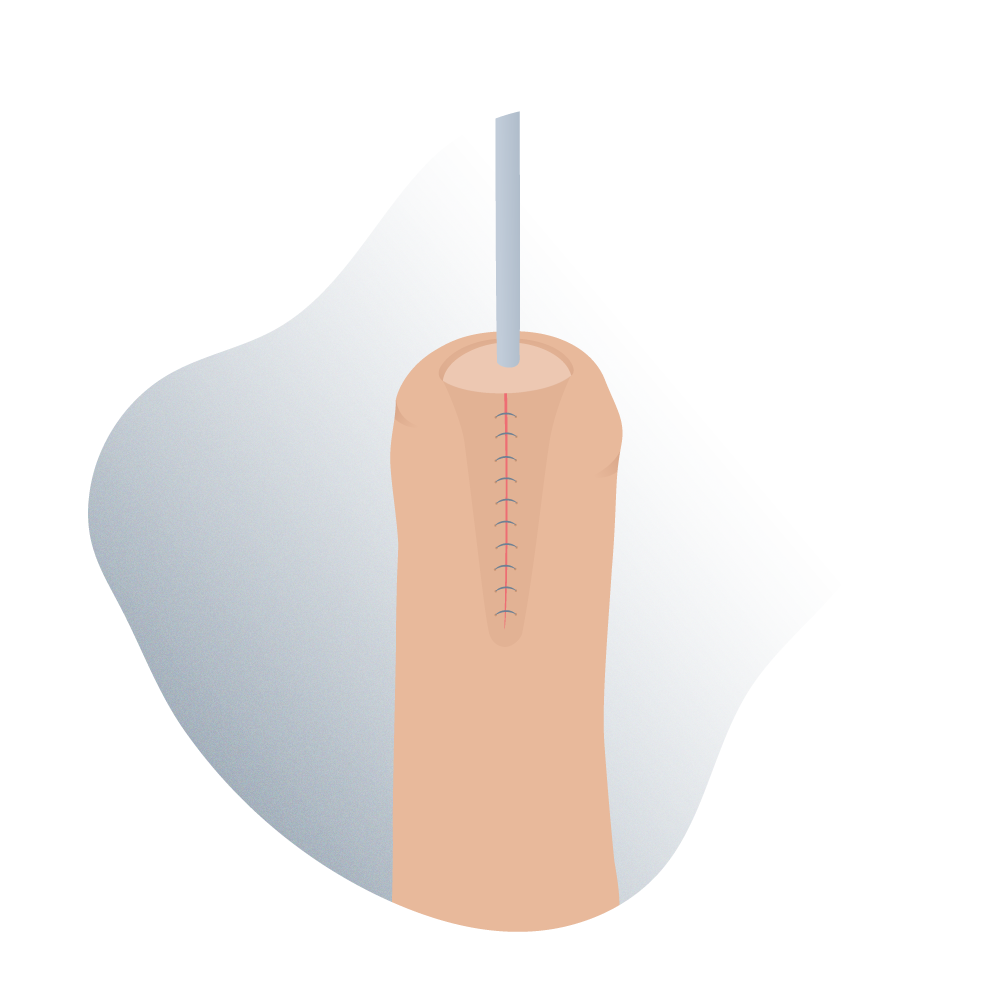
Hypostasia surgery 03
Regardless of the technique chosen to repair the hypospadias, it should include the following points:
The treatment of the penis curve
Reconstruction of the urethra, meatus, and glans
Cutaneous coverage of the penis
Hypostasia surgery 04
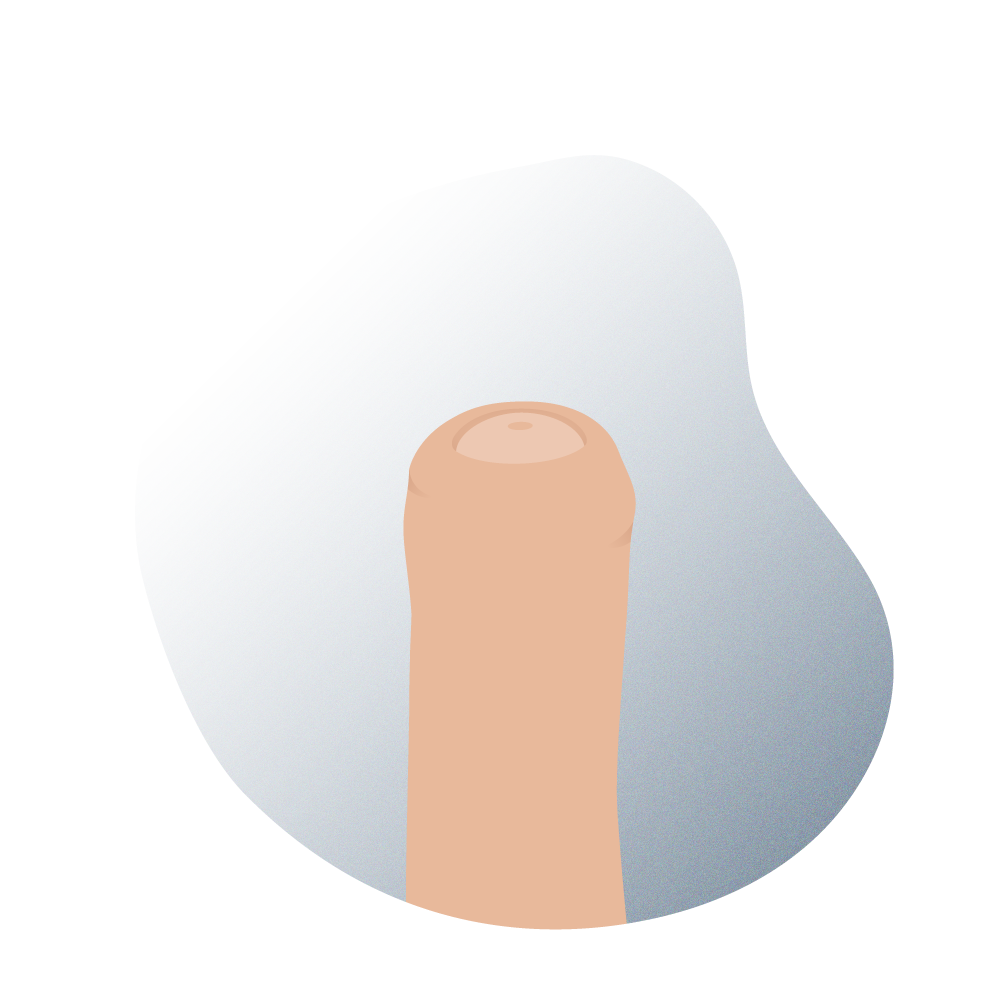
Hypostasia surgery 05
Solutions
Most common complications, problems, and solutions
Infection and the formation of a hematoma or an ischemic flap can lead to poor healing and produce a fistula or partial crack on the repair. Fortunately, it’s rare to lose the repair completely, but we will have to perform the surgery again when the tissues are completely cured (not before 6 months) if it happens. The results of hypospadias surgery reflect the severity of the original defect, the type of technique used, and the experience of the surgeon.
- Fistula
- Meatal stenosis
- Urethral stenosis
- Persistent curvature
- Urethrocele or urethral ballooning
Fistulas are undoubtedly the most common complications after hypospadias surgery. They may appear immediately after removal of the urethral catheter or years after surgical repair. The location of the fistula varies, but it is always close to the glans or at the anastomosis of the neourethra with the native urethra. Before its repair, it is important to exclude the presence of meatal stenosis and/or any other problem that increases the risk of recurrence. The fistula repair should not be underestimated since it accounts for up to 50% of recurrence in some cases. It is advisable to wait for at least 6 months after the original repair before closing the fistula.
It can create urination difficulties, a thin urine stream, and urinary tract infection in some patients, as well as incomplete bladder voiding. Mild stenosis can be treated on an outpatient basis with dilatations. When the stenosis is severe, dilatation is needed under general anesthesia and even meatotomy.
When it occurs, it’s always at the distal or proximal end of the neourethra. Distal stenosis is usually accompanied by fistula and proximal stenosis and is a serious complication that often requires resection of the stricture either endoscopically or openly.
Generally, this occurs if the initial correction wasn’t quite successful, although postoperative fibrosis can also influence it. Surgery to bend the tunica albuginea upwards is usually enough to correct it.
This is the dilation of the proximal urethra, sometimes secondary to distal stenosis. It can also occur due to the absence of spongy tissue thus hindering the support of the neourethra as is the case in tubularized urethroplasty with a Duckett type preputial flap. It can cause post-void dribbling or even a urethral calculus due to urinary stasis, in which case the exeresis of redundant urethral tissue and/or distal stenosis would be required.
Frequently asked questions at the Andromedi centres in Madrid, Seville and Tenerife
Hide
Some cases of hypospadias may reappear a few months after being operated on, with the appearance of fistulas usually the main setback. It is possible to re-intervene with a good prognosis in most of such cases, but we must always assess the patient’s condition carefully because each new intervention adds instability in the tissues of the affected area. You can only enter the operating room again after a substantial period of time and the reasons why the previous one was not successful must be well analyzed. This explains why the knowledge and analytical capacity of an experienced team such as ours are basic aspects to be taken into account by the parents. In other words, it is a surgery that must be performed by a medical team of proven ability.
In Spain, all the cases usually have public medical coverage by the state or regional service. However, there are many parents who prefer to go to private medical centers (whether they have medical insurance or not) regardless of the price. This choice which often involves a cost on the family finances is usually guided by two main reasons. The first is the freedom to choose the professional doctor and the second is to shorten the waiting periods which are sometimes quite lengthy. Both are important issues to take into account since the successful correction of hypospadias depends a lot on the expertise and experience of the surgeon, and it is a condition that needs to be addressed with some urgency i.e. in the first months of the child’s life (before 15 months).
After a well planned and executed intervention, the resulting phalloplasty leaves the penis of the child without any present or future sexual or urinary problems. So, it is perfectly prepared for its development at puberty without any type of sequela. This further highlights the importance of choosing the surgical team since it is a very sensitive operation that could end up with setbacks in the future if not executed perfectly.
Author
Natalio Cruz MD, with 25 years of medical experience, has been until 2016 Head of the Andrology Unit in the Urology Service of the Virgen del Rocío Hospital in Seville, National Coordinator of Andrology in the Spanish Association of Urology (AEU) and General Secretary in the ESSM, positions that he has narrowed to focus squarely on this exciting project of offering a high-level private medical consultation in Marbella, Seville, Madrid and Tenerife.
Andromedi pertenece a las organizciones médicas más destacadas en el sector de la Uro-Andrología