
Diagnosis
Diagnosis of urethral stricture

The most common form of presentation is obstructive symptoms of the lower urinary tract, ranging from a decrease in the caliber of the voiding stream to acute or chronic urinary retention. It can also start with a urinary tract infection, prostatitis, or epididymitis. Frequently, the patient presents a decrease in the force of the jet progressively over a long time, to which he becomes accustomed. It is well tolerated until the appearance of some complication.
The suspected diagnosis is essential, especially in older patients, in whom the symptoms are attributed to prostate disease, although they do not improve with medical treatment, and the problem arises during access to the bladder during the intervention.
All male patients evaluated for obstructive symptoms in the urinary tract (whatever their type) should have a complete medical history in the to be investigated:
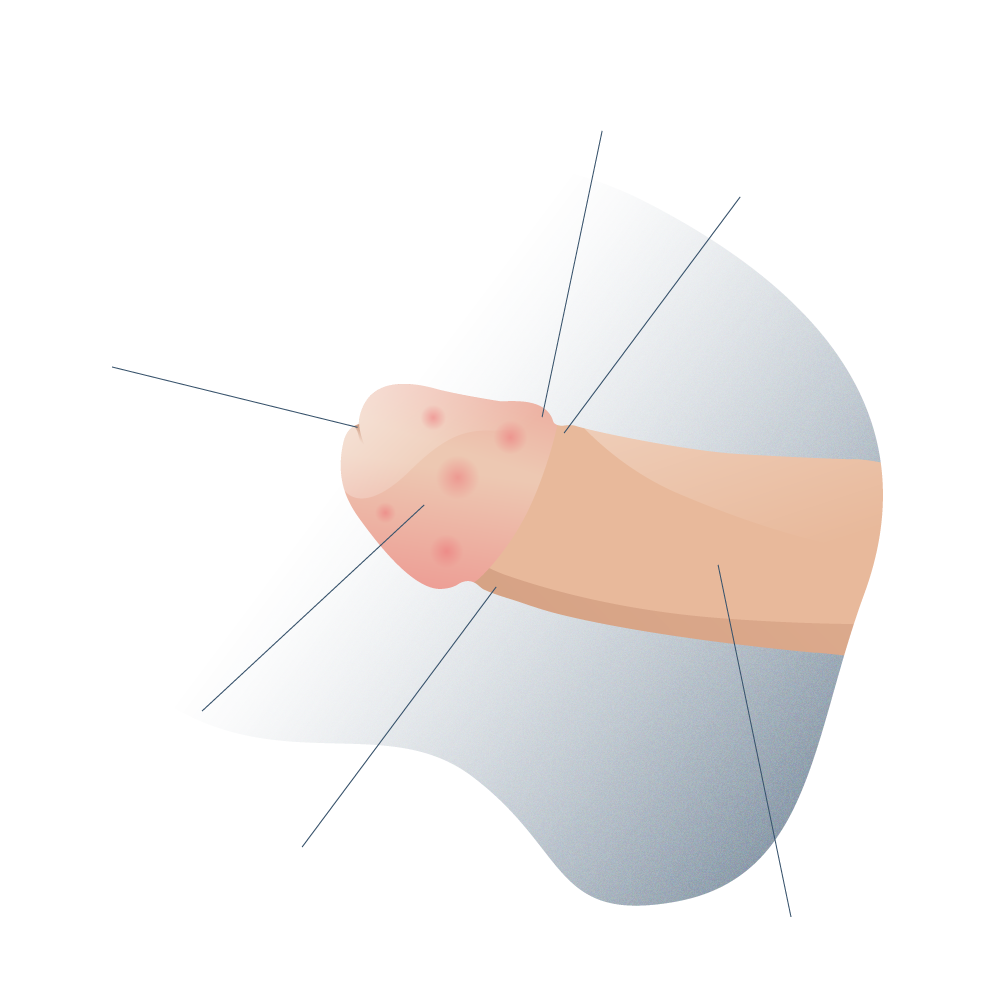
- Previous episodes of urinary tract infections (UTI) that may have generated scarring processes that obstruct the urethra (this phenomenon is known as spongiofibrosis).
- History of sexually transmitted infections (STIs) with special emphasis on gonorrhea and chlamydia.
- Previous use of urinary catheters, in men undergoing surgery or with bladder problems.
- History of prostate surgery or penis enlargement.
- Traumas or blows in the genital and perineal area.
Some pathologies such as diabetes mellitus, certain cardiovascular diseases or habits such as smoking can significantly predispose to the appearance of exaggerated scar tissue on the walls of the urethra and lead to partial or total stenosis.
It is important to know the state of the erectile function of the penis and the quality of the ejaculations. Some men with partial urethral stricture may have difficulty conceiving a child.
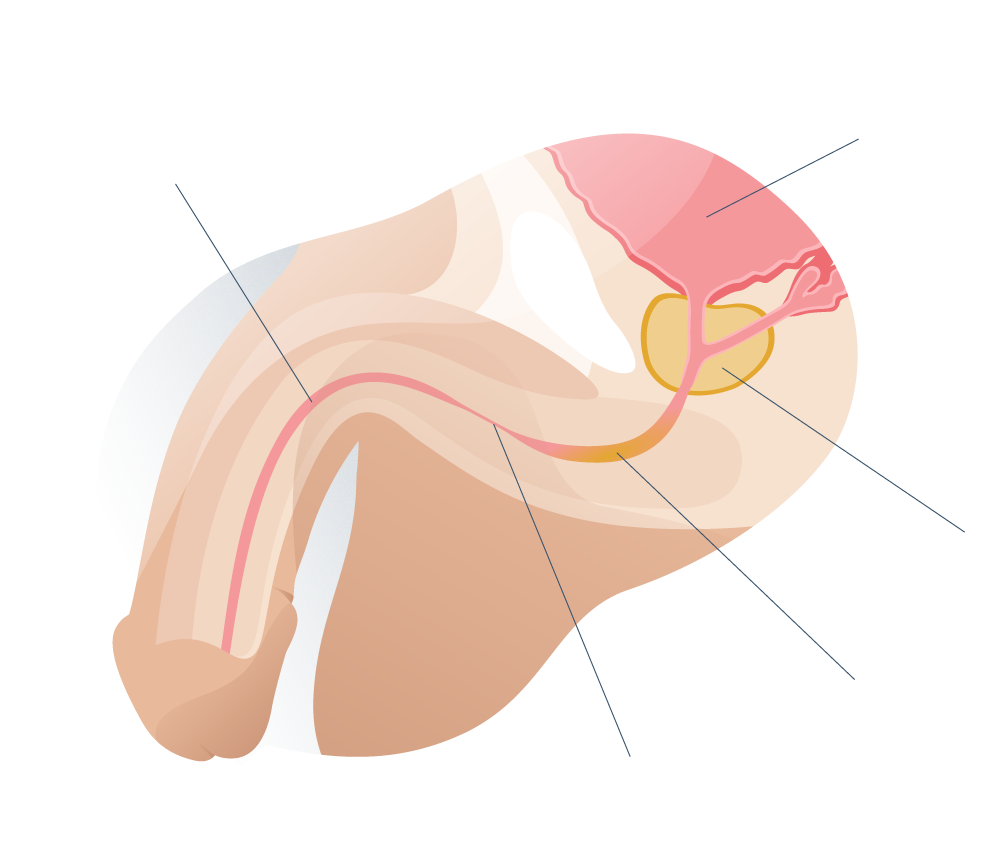
To choose an appropriate technique for the surgical treatment of urethral stricture, it is necessary to know the following information regarding it:
- Length. Longer urethras are more prone to mechanical obstruction than shorter urethras.
- Number of strictures. It is common to find that the points of narrowing are several and not one as is usually thought. These multiple obstructions usually have longer treatments and more rigorous medical surveillance, to avoid the development of complications.
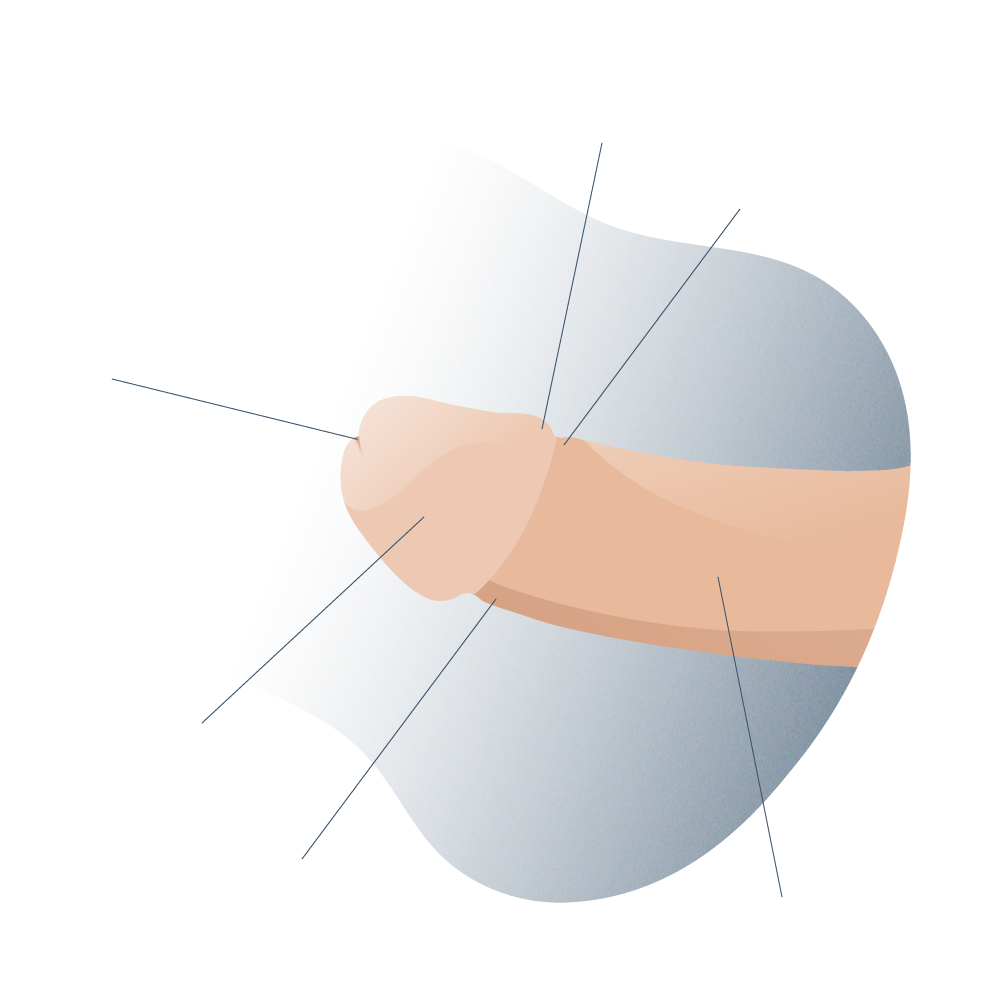
- Location of the stenosis. The urethra is divided into seven segments and each of them can be compressed for different reasons and alter urinary function to a greater or lesser extent. the most frequent site of urethral narrowing (with 40% of cases) is the urethral segment, at the root of the erectile member.
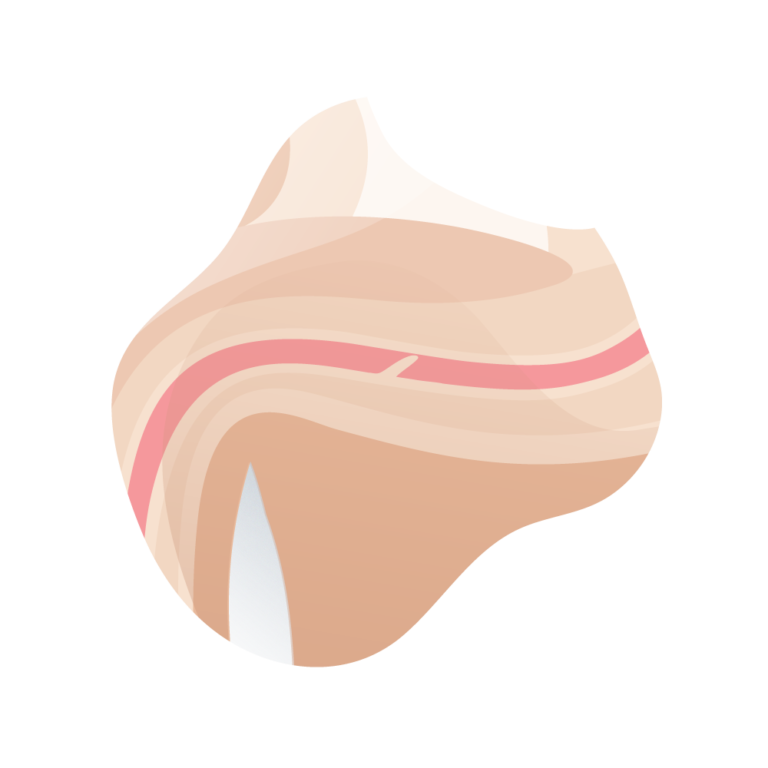
- Degree of spongiofibrosis. The scarring processes of the urethral tissue can lead to partial or total obstruction of the urinary duct (narrowing) and, in the medical evaluation, it is important to determine the degree of spongiofibrosis to anticipate the appropriate surgical conduct.
The first three data can be known by one or more of the following techniques. However, the association of several of them is usually recommended to adequately plan the approach route and the surgical technique.
Ideally, it should be done with a thin rigid cystoscope, with a 0-30 ° optics, or with a flexible cystoscope. In addition to being able to perform an approximate calibration, the appearance of the urethral mucosa can be seen. The whiter it is, the more it points to a higher degree of spongiofibrosis.
- Uretroscopia
- Uretrografía retrógrada y miccional
- Calibrado uretral
- Ecografía
- Flujometría
Lo ideal es realizarla con un cistoscopio rígido fino, con óptica de 0-30° o con un cistoscopio flexible. Además de poder realizar un calibrado aproximado, se puede ver el aspecto de la mucosa uretral. Cuanto más blanquecina es, más apunta a un mayor grado de espongiofibrosis.
Es recomendable realizar esta técnica bajo la supervisión de un urólogo. En ese momento o previamente (con una sonda muy fina o a través de talla suprapúbica) se deberá haber llenado la vejiga de contraste. Consiste en la realización de radiografías en diferentes proyecciones oblicuas anteriores pélvicas previa introducción de contraste por uretra desde la fosa navicular de forma retrógrada. De ese modo, podremos obtener imágenes de llenado retrógrado, imágenes miccionales e, incluso, imágenes de uretrografía combinada con intento miccional a la vez del llenado retrógrado.
Se realiza con bujías de bola y es muy útil en estenosis distales. Tiene la limitación de que en caso de estenosis largas o múltiples no es muy valorable, ya que la más distal suele condicionar el estudio de las más proximales.
No se suele utilizar debido a que exigen un ecografista con experiencia y los resultados son habitualmente no concluyentes.
Una curva obstructiva con morfología «en meseta» apunta hacia una estenosis de uretra.
El grado de espongiofibrosis suele apreciarse realmente durante la intervención, aunque puede sospecharse de forma aproximada mediante el aspecto uretral durante la endoscopia, la mala distensión durante la misma, cuando se realiza la uretrografía retrógrada, por la existencia de manipulaciones o intervenciones previas y, eventualmente, en la ecografía.



Andromedi pertenece a las organizciones médicas más destacadas en el sector de la Uro-Andrología